Why Antipsychotics Can Change Your Body in Ways You Didn’t Expect
Antipsychotic medications save lives. For people with schizophrenia, bipolar disorder, or severe psychosis, these drugs can mean the difference between isolation and stability. But there’s a hidden cost many don’t talk about: metabolic risks. These aren’t just side effects-they’re serious, sometimes life-threatening changes to how your body processes sugar, fat, and energy. And they start quietly, often before you even notice weight gain.
Second-generation antipsychotics (SGAs), the most commonly prescribed today, carry a much higher risk of metabolic problems than their older counterparts. Studies show that 32% to 68% of people taking these drugs develop metabolic syndrome-a cluster of conditions including belly fat, high blood pressure, high triglycerides, low good cholesterol, and elevated blood sugar. Compare that to just 3.3% to 26% in people not taking antipsychotics. That’s not a small difference. It’s a tripled risk of heart disease and stroke.
Which Antipsychotics Are Most Likely to Cause Weight Gain and Blood Sugar Spikes?
Not all antipsychotics are created equal when it comes to metabolic damage. Some are far safer than others, and knowing the difference can change your treatment plan.
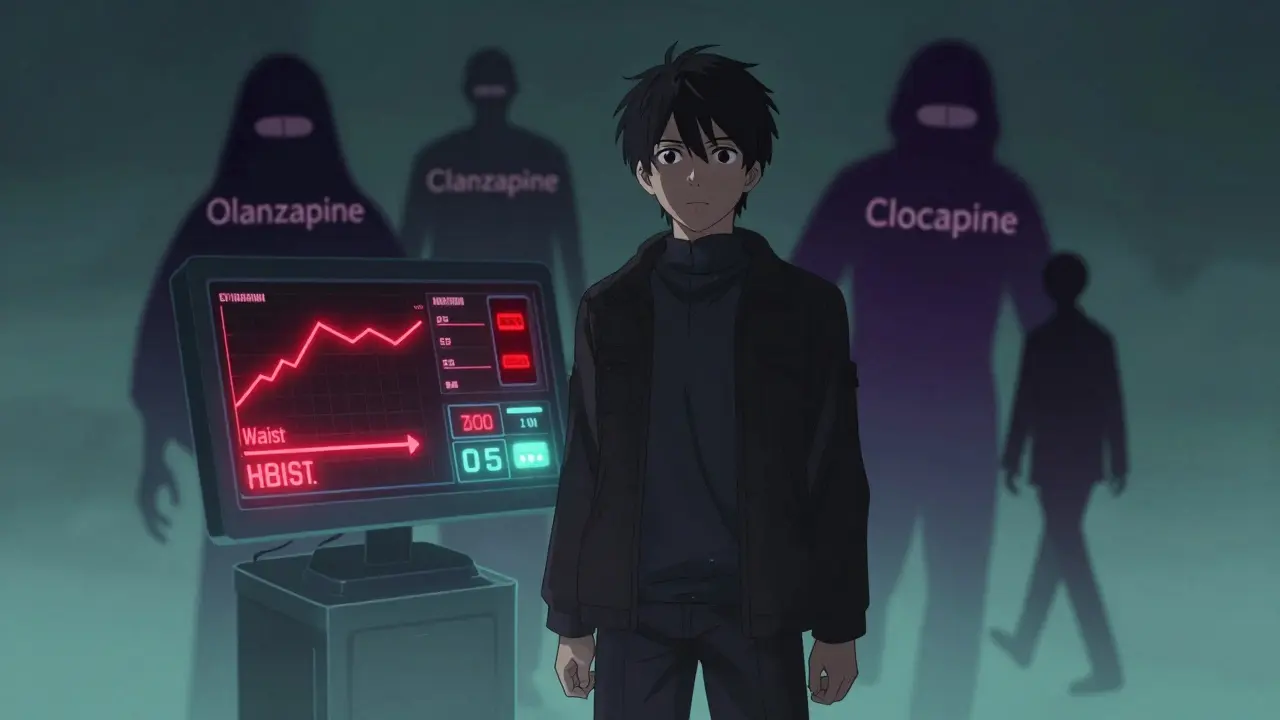
- Olanzapine and clozapine are the worst offenders. In the CATIE study, people on olanzapine gained an average of 2 pounds per month. Nearly 30% experienced major weight gain over 18 months. Both also spike blood sugar and triglycerides significantly.
- Quetiapine, risperidone, asenapine, and amisulpride fall in the middle-they cause noticeable but less extreme changes.
- Ziprasidone, lurasidone, and aripiprazole are the best choices if metabolic health is a concern. These drugs have minimal impact on weight and blood sugar, making them ideal for patients already at risk for diabetes or heart disease.
It’s not just about the drug itself. Genetics, diet, activity level, and even how long you’ve been on the medication all play a role. But the drug class you’re on sets the baseline risk.
How Antipsychotics Disrupt Your Metabolism (Even Before You Gain Weight)
Many assume weight gain is the main problem. But the real danger starts earlier-before the scale moves.
These drugs interfere with how your body regulates energy at a cellular level. They affect the hypothalamus (your brain’s hunger and metabolism control center), reduce insulin sensitivity in muscle and fat tissue, and mess with how your liver handles fats and glucose. Some even damage pancreatic beta cells, which produce insulin.
Research shows metabolic changes-like rising blood sugar or triglycerides-can appear within weeks of starting treatment, even if you haven’t gained a pound. That’s why waiting until you notice weight gain to check your health is too late. By then, damage may already be underway.
The Real Danger: Metabolic Syndrome and Early Death
Metabolic syndrome isn’t just a label. It’s a ticking clock. People with this condition have three times the risk of heart attack and stroke compared to those without it. In one study with a median follow-up of nearly 7 years, those with metabolic syndrome had significantly higher rates of death from cardiovascular causes.
For people on antipsychotics, this isn’t theoretical. They’re already at higher risk for metabolic issues just because of their illness. Psychosis itself is linked to poor diet, inactivity, and smoking. Add antipsychotics into the mix, and the risk skyrockets. The result? People with serious mental illness die 10-20 years earlier than the general population-mostly from preventable heart disease and diabetes.
What Needs to Be Monitored-and When
Guidelines from the American Psychiatric Association and the American Diabetes Association are clear: every patient starting an antipsychotic must be monitored for metabolic changes. But in practice, too many doctors skip this step.
Here’s what you need checked, and when:
- Before starting: Weight, BMI, waist circumference, blood pressure, fasting blood glucose, and lipid panel (cholesterol and triglycerides).
- At 4 weeks: Weight and blood pressure. If anything’s off, check glucose and lipids.
- At 12 weeks: Full metabolic panel again.
- At 24 weeks: Repeat full panel.
- Every 3 to 12 months after that: Depends on your risk. High-risk patients (like those on olanzapine or with pre-diabetes) need checks every 3 months. Stable patients on safer drugs can go every 6-12 months.
Waist measurement matters more than weight. A waist over 40 inches in men or 35 inches in women signals dangerous belly fat-even if your BMI is normal.
What to Do If Your Numbers Start Rising
Getting bad news from a blood test doesn’t mean you have to stop your medication. It means you need a plan.
Start with lifestyle changes: A structured diet and exercise program can cut metabolic risks by up to 50%. You don’t need to run marathons. Just 150 minutes a week of brisk walking, plus cutting out sugary drinks and processed carbs, makes a real difference.
Consider switching meds: If you’re on olanzapine or clozapine and your glucose or cholesterol is climbing, talk to your psychiatrist about switching to a lower-risk drug like lurasidone or aripiprazole. This isn’t giving up-it’s protecting your long-term health. For people with treatment-resistant psychosis, clozapine may still be necessary. But even then, you can add medications like metformin to help control blood sugar.
Use supportive tools: Many clinics now offer integrated care-psychiatrists working with dietitians, exercise physiologists, and diabetes educators. These programs improve both mental and physical health outcomes.
Why So Many Patients Stop Taking Their Medication
One of the biggest reasons people with schizophrenia or bipolar disorder stop taking their antipsychotics? Weight gain.
Studies show 20% to 50% of patients discontinue treatment because of metabolic side effects. And when they do, relapse rates jump. Hospitalizations follow. It’s a vicious cycle: the drug keeps psychosis at bay, but it also makes you feel worse physically-so you stop taking it, and your mental health crashes.
This isn’t about willpower. It’s about having the right support. If your doctor doesn’t talk to you about weight gain before you start the drug, or doesn’t check your numbers regularly, you’re being set up to fail.
Long-Acting Injections Don’t Solve the Problem
Some people think switching to long-acting injectable (LAI) antipsychotics will reduce metabolic risks. It won’t. The drug is still the same. Whether you swallow a pill or get a shot every two weeks, your body still processes it the same way. Monitoring is just as critical.
What You Can Do Right Now
If you’re on an antipsychotic:
- Ask your doctor for your last metabolic panel results.
- Know your numbers: weight, waist, blood pressure, fasting glucose, triglycerides, HDL.
- If you don’t have a record of these tests in the last 6 months, request them.
- Ask: “Is this the safest antipsychotic for my body?”
- Don’t wait for symptoms. Ask for a dietitian referral or a walking program.
If you’re a caregiver or family member: Help track appointments. Bring a notebook to visits. Ask the same questions. You’re not overstepping-you’re helping save a life.
The Bottom Line
Antipsychotics are essential for many. But they’re not harmless. The metabolic risks are real, well-documented, and preventable. The key isn’t avoiding these drugs-it’s managing them wisely. Regular monitoring, early intervention, and choosing the right medication for your body can let you stay stable mentally while protecting your heart, liver, and pancreas. You deserve both.
Do all antipsychotics cause weight gain?
No. While many second-generation antipsychotics do cause weight gain, some have much lower risks. Olanzapine and clozapine are the worst offenders, while ziprasidone, lurasidone, and aripiprazole are far less likely to cause significant weight gain or metabolic changes. The choice of medication should factor in your personal health risks.
How soon after starting an antipsychotic do metabolic changes begin?
Metabolic changes can begin within the first few weeks, often before any noticeable weight gain. Blood sugar and triglyceride levels may rise even if your weight stays the same. That’s why early monitoring-at 4 and 12 weeks-is critical.
Can I reverse metabolic damage caused by antipsychotics?
Yes, in many cases. Losing even 5-10% of body weight can significantly improve blood sugar, cholesterol, and blood pressure. Lifestyle changes-diet, exercise, quitting smoking-are the most effective tools. In some cases, adding metformin or other medications can help reverse insulin resistance. The earlier you act, the better your chances.
Should I stop my antipsychotic if I gain weight?
Never stop suddenly. Stopping antipsychotics without medical supervision can lead to relapse, hospitalization, or worse. Instead, talk to your psychiatrist. They can help you adjust your treatment-whether that means switching to a safer drug, adding a metabolic medication, or starting a structured weight management program.
Are there any tests I should ask for regularly?
Yes. Ask for: weight and waist measurement, blood pressure, fasting blood glucose, and a lipid panel (total cholesterol, triglycerides, HDL, LDL). These should be checked before starting the medication, then at 4, 12, and 24 weeks, and every 3-12 months after that depending on your risk level.
Does taking antipsychotics increase my risk of diabetes?
Yes, significantly. People on second-generation antipsychotics are two to three times more likely to develop type 2 diabetes than the general population. The risk is highest with olanzapine and clozapine. Regular glucose monitoring and early lifestyle changes can reduce this risk.
Can exercise help reduce the metabolic side effects?
Absolutely. Regular physical activity improves insulin sensitivity, lowers triglycerides, raises HDL cholesterol, and helps control weight-even without major weight loss. Aim for 30 minutes of brisk walking five days a week. Even small increases in movement make a measurable difference in metabolic health.
Why don’t more doctors monitor metabolic health in patients on antipsychotics?
Despite clear guidelines from major medical associations, many clinicians lack time, training, or systems to track metabolic health. Mental health care is often separated from physical health care, and metabolic monitoring isn’t always prioritized. Patients need to advocate for themselves-ask for the tests, request referrals, and don’t accept silence as an answer.

Comments
Grace Rehman
so we're just supposed to accept that our brains are being rewired by pills that also slowly kill our hearts? like... cool. guess i'll just keep my diabetes and my psychosis in balance. nobody ever said mental health care was about living longer, right?
also why is the word 'metabolic' in every other sentence? sounds like a pharmaceutical ad.
On December 20, 2025 AT 22:39
Jerry Peterson
this is actually one of the most practical posts i've seen on here. i'm on risperidone and my doc never checked my lipids until i asked. turned out my triglycerides were through the roof. switched to lurasidone last year and my numbers are back to normal. no magic, just listening to the science.
On December 21, 2025 AT 13:51
Hannah Taylor
they dont want you to know but the FDA is in bed with big pharma and theyre using antipsychotics to depopulate the poor. weight gain? its not side effect its a feature. they want you fat and diabetic so youll need more meds and youll die sooner and save the government money on social security. i saw it on a video. the numbers dont lie.
On December 21, 2025 AT 20:55
Jason Silva
bro this is real. i was on olanzapine for 2 years. gained 70lbs. got prediabetic. my heart was pounding like a drum. switched to aripiprazole and now i can run 5k without gasping. 🙌 life changed. dont let em fool you. your body is not a lab rat.
On December 22, 2025 AT 14:32
mukesh matav
interesting. i'm on quetiapine in India. doc just gives script, no tests. family says 'you look good' so they think it's fine. but i feel slow. tired. like my insides are syrup. maybe i should ask for bloodwork. but who has time?
On December 24, 2025 AT 03:35
Peggy Adams
ugh i just don't care anymore. i take my pill. i gain weight. i eat chips. i'm tired. my doctor says 'just exercise' like i'm not already fighting to get out of bed every day. why is it always my fault?
On December 25, 2025 AT 12:00
Sarah Williams
you are not alone. this is fixable. ask for the tests. ask for the switch. ask for the dietitian. your life matters more than the stigma. you deserve to be stable AND healthy.
On December 26, 2025 AT 08:15
Theo Newbold
the data is solid but the framing is naive. you assume patients have access to specialists, time off work, insurance coverage, and the cognitive capacity to advocate for themselves. for most, this is a luxury. the system is designed to ignore metabolic decline until it's irreversible. this post is a Band-Aid on a hemorrhage.
On December 26, 2025 AT 21:30
Jay lawch
in India we know the truth. america pushes these drugs because they want to control the mind and break the spirit. the west uses antipsychotics as chemical handcuffs. they don't care if you live or die, only if you obey. i read a paper once - it said 87% of patients on these drugs are from lower income groups. coincidence? no. it's colonial medicine. we must wake up.
On December 27, 2025 AT 04:02
Christina Weber
There is a critical omission in this post: the distinction between correlation and causation. While metabolic syndrome is more prevalent among patients on SGAs, it is also more prevalent among individuals with severe psychiatric illness due to lifestyle factors, genetic predisposition, and socioeconomic determinants. To attribute the entire risk to the medication is scientifically misleading and potentially dangerous.
On December 28, 2025 AT 01:43
Cara C
i just want to say thank you for writing this. i’ve been scared to ask my doctor about switching meds because i thought i was being ‘difficult.’ but now i’m going to bring this list with me to my next appointment. i don’t want to lose my mind or my heart. i want both.
On December 29, 2025 AT 00:08
Michael Ochieng
this is gold. i work in a community clinic and we just started a program where our psych nurses do metabolic checks during med refills. patients are shocked at first but then they’re grateful. one guy said 'no one ever asked me about my waist size before.' we’re not fixing the system, but we’re making tiny cracks in the wall.
On December 30, 2025 AT 19:41