Chronic kidney disease (CKD) doesn’t announce itself with pain or sudden symptoms. It creeps in silently, often for years, while your kidneys slowly lose function. By the time you feel tired, swollen, or notice changes in urination, it’s often too late to reverse the damage. But here’s the truth: chronic kidney disease can be caught early - and when it is, progression can be stopped in its tracks. Most people with CKD don’t know they have it. In the U.S., about 1 in 7 adults have it. Yet only 1 in 10 are diagnosed. That’s not because doctors aren’t looking - it’s because they’re looking in the wrong way.
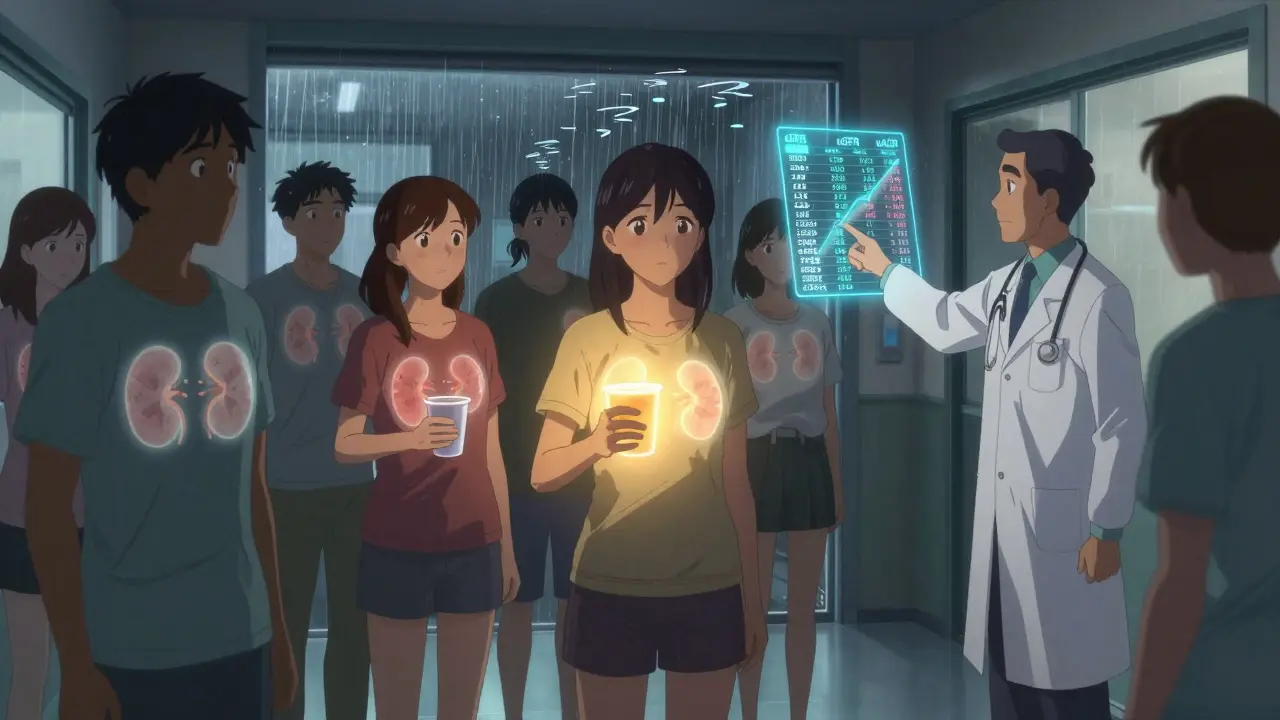
Why Two Tests Are Non-Negotiable
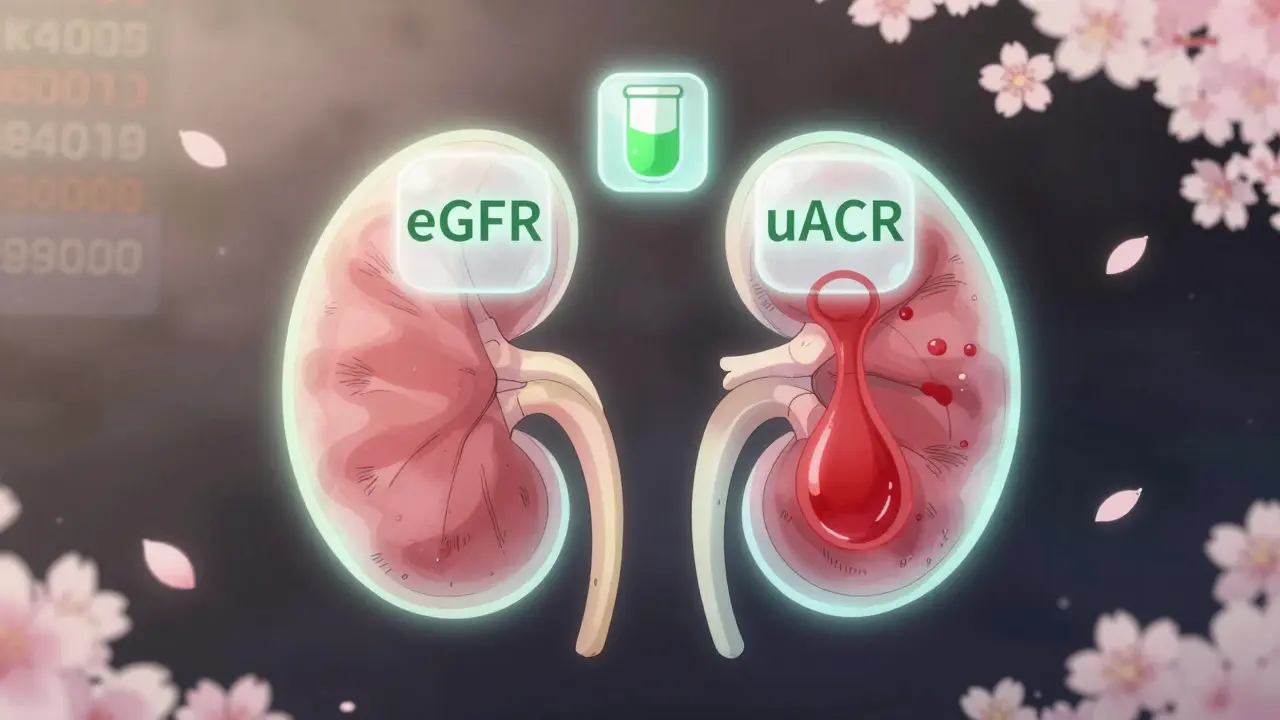
For decades, doctors checked one thing: serum creatinine. If it was normal, they assumed the kidneys were fine. But creatinine is unreliable. It varies with muscle mass, age, diet, and race. A healthy 80-year-old woman with low muscle mass can have a normal creatinine level while her kidneys are already failing. Meanwhile, a young athlete with high muscle mass might have a high creatinine - even with perfect kidney function. The real diagnostic standard now requires two tests: eGFR and uACR. Neither one alone is enough. You need both. eGFR - estimated glomerular filtration rate - tells you how well your kidneys are filtering waste. It’s calculated using your creatinine, age, sex, and race. But here’s the catch: if your eGFR is 65, and you have diabetes, you’re not off the hook. That’s still stage 2 CKD if your uACR is high. uACR - urine albumin-to-creatinine ratio - measures protein leaking into your urine. Healthy kidneys don’t let protein escape. When they do, it’s an early red flag. A uACR of 30 mg/g or higher means kidney damage is happening, even if your eGFR is still normal. This two-test rule isn’t optional. It’s the foundation of modern CKD diagnosis. Skipping one test means missing up to 40% of early cases. And that’s not speculation - it’s from the 2018 National Health and Nutrition Examination Survey.Stages of CKD: What Your Numbers Really Mean
CKD is broken into five stages. But stages 1 and 2 are where the game changes.- Stage 1: eGFR ≥90, but uACR ≥30 mg/g. Your kidneys are still filtering well, but they’re leaking protein. Damage is present.
- Stage 2: eGFR 60-89, uACR ≥30 mg/g. Slight decline in function, but still plenty of time to act.
- Stage 3a: eGFR 45-59. Mild to moderate loss. This is where many people are diagnosed - too late.
- Stage 3b: eGFR 30-44. Moderate to severe loss. Complications like anemia and bone disease start appearing.
- Stage 4: eGFR 15-29. Severe loss. Preparation for dialysis or transplant begins.
- Stage 5: eGFR <15. Kidney failure. Dialysis or transplant required.
Who Should Be Screened - And How Often
Screening isn’t for everyone. It’s for those at risk. And the risk factors are clear:- Diabetes (type 1 or 2)
- High blood pressure
- Family history of kidney failure
- Heart disease
- Obesity
- African American, Native American, or Hispanic heritage
- Chronic use of NSAIDs (like ibuprofen) or certain antibiotics
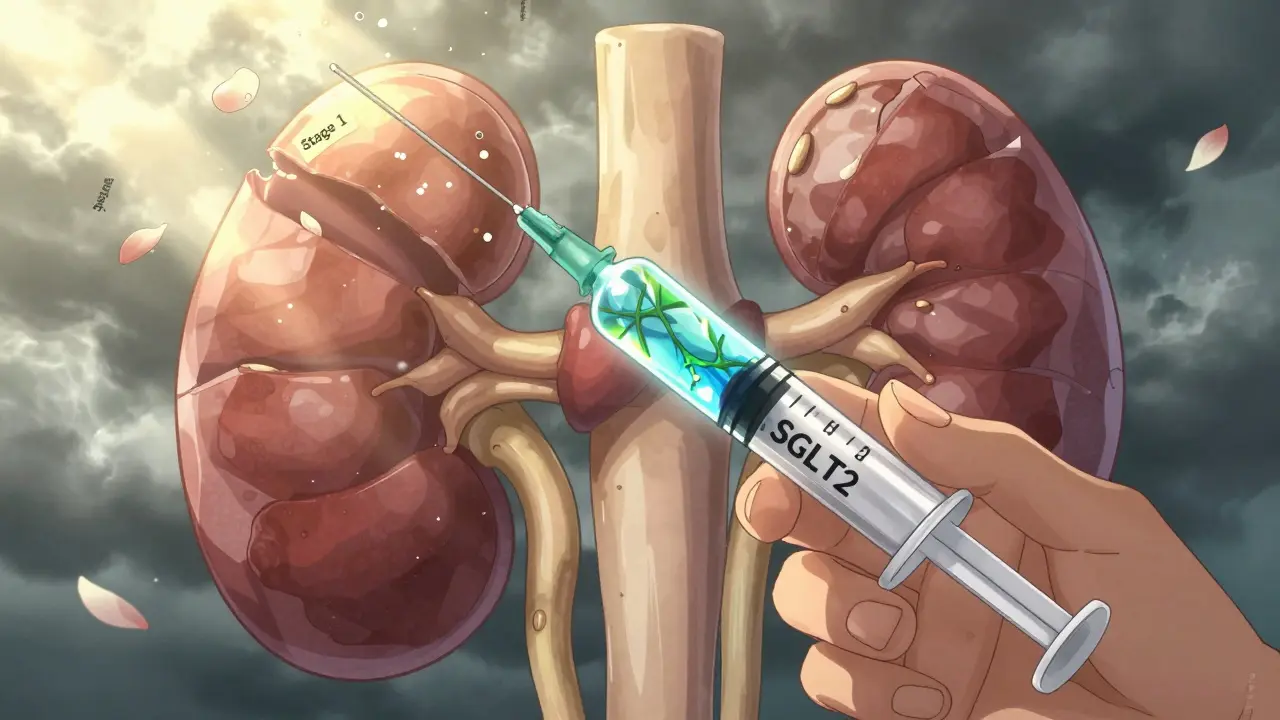
What Actually Works to Slow Progression
Finding CKD early is only half the battle. The other half is doing something about it. The most proven tools:- Blood pressure control: Target <130/80 mmHg. The SPRINT trial showed this cuts progression risk by 27% compared to the old target of <140/90.
- SGLT2 inhibitors: Originally diabetes drugs, these now prevent kidney failure in CKD patients with proteinuria. The CREDENCE trial showed a 32% reduction in progression to end-stage kidney disease.
- ACE inhibitors or ARBs: These lower blood pressure and reduce protein leakage. They’re first-line for CKD patients with albuminuria.
- Dietary changes: Reduce salt, avoid processed foods, limit protein if your eGFR is below 45. A 2022 meta-analysis showed that structured dietary counseling reduced annual eGFR decline from 3.5 to 1.2 mL/min/1.73 m².
Why So Many Doctors Still Miss It
You’d think with clear guidelines, this would be routine. But it’s not. A 2022 study in the Annals of Internal Medicine found only 52.7% of primary care providers consistently order both eGFR and uACR. In rural areas? It drops to 32%. Why?- Electronic health records don’t prompt for both tests.
- Doctors think “normal creatinine” means normal kidneys.
- They don’t know how to interpret the combination.
- They assume patients won’t follow up.
What’s Changing in 2025 and Beyond
The tide is turning - slowly. The FDA cleared the first AI tool for CKD risk prediction in May 2023. NephroSight by Renalytix analyzes 32 clinical variables - from lab results to medication history - to flag high-risk patients before their eGFR drops. It’s already being piloted in VA hospitals. In 2023, the Biden administration launched a $150 million initiative to require dual testing in all Federally Qualified Health Centers by 2026. That’s 1.2 million people who could be diagnosed early. The biggest controversy? Race adjustment in eGFR calculations. For years, labs automatically added 15% to eGFR for Black patients, assuming they had more muscle mass. But that masked early disease. Removing race adjustment could increase early detection in African Americans by 12.3%, according to 2024 KDIGO preliminary data. Point-of-care uACR devices are coming. By 2025, you might get your protein test done in your doctor’s office in 10 minutes - no lab needed. The Veterans Health Administration saw screening rates jump 40% with these devices.What You Can Do Today
If you have diabetes, high blood pressure, or a family history of kidney disease:- Ask for both eGFR and uACR - don’t accept just creatinine.
- If your uACR is over 30, ask why. Ask what’s next.
- Keep your blood pressure under 130/80.
- Stop taking ibuprofen or naproxen daily without medical supervision.
- Get a visual of your CKD stage. A 2023 National Kidney Foundation survey found patients who saw their stage on a chart were 28% more likely to stick to their treatment plan.
Can chronic kidney disease be reversed?
In early stages (1 and 2), CKD progression can often be stopped or significantly slowed with medication, blood pressure control, and lifestyle changes. While existing damage may not fully reverse, the kidneys can stabilize and continue functioning normally for many years. Once you reach stage 4 or 5, the damage is usually permanent, and treatment shifts to slowing decline and preparing for dialysis or transplant.
Is a urine test enough to diagnose CKD?
No. A urine test (uACR) can show kidney damage, but it doesn’t measure how well your kidneys are filtering. You also need an eGFR - calculated from a blood test - to determine kidney function. Both tests together are required for a confirmed diagnosis of CKD. Relying on just one test misses up to 40% of early cases.
Why do some people get CKD even with normal blood pressure and no diabetes?
CKD can be caused by genetics, autoimmune diseases like lupus, chronic infections, long-term use of certain medications (like NSAIDs), or even unknown causes. Family history is a major risk factor - if a close relative had kidney failure, your risk goes up. That’s why screening is recommended for anyone with a family history, regardless of other conditions.
Does drinking more water help prevent CKD?
Staying hydrated supports kidney function, but drinking extra water won’t prevent or reverse CKD if you already have damage. For people with early CKD, overhydration can even be harmful if they have fluid retention. The key isn’t quantity - it’s avoiding dehydration and limiting substances that stress the kidneys, like salt, sugar, and processed foods.
Are over-the-counter painkillers safe if I have CKD?
No. Common NSAIDs like ibuprofen, naproxen, and aspirin can reduce blood flow to the kidneys and worsen function, especially in early CKD. Acetaminophen (Tylenol) is generally safer, but even that should be used carefully and only as directed. Always check with your doctor before taking any pain reliever regularly.
How often should I get tested if I’m at risk?
If you have diabetes, get both eGFR and uACR tested every year. If you have high blood pressure, test at least once a year - or every 6 months if your blood pressure is hard to control. If you have a family history of kidney failure or are African American, Native American, or Hispanic, ask your doctor to include these tests in your annual checkup - even if you feel fine.

Comments
mike swinchoski
This is why people die early. Everyone just waits till they’re falling apart. Doctors don’t care. They just write prescriptions and send you on your way. You think your creatinine is fine? That’s a lie. Your kidneys are already screaming and you’re sipping your coffee like nothing’s wrong.
On January 12, 2026 AT 17:39
jefferson fernandes
Let me be clear: eGFR alone is a trap. It’s like judging a car’s engine by how loud it sounds-ignoring the oil pressure, the coolant, the belts. You need uACR. Period. If your doctor skips it, find a new one. This isn’t optional medicine-it’s survival. And if you’re diabetic? You’re already on the clock. Don’t wait for the alarm to go off.
On January 13, 2026 AT 05:32
Acacia Hendrix
Frankly, the reliance on eGFR is a relic of 20th-century medical dogma. The uACR paradigm represents a paradigm shift grounded in proteomic biomarker kinetics and glomerular permeability dynamics. Without this dual-analyte framework, we’re essentially practicing nephrology with a blindfold. It’s not just about detection-it’s about epistemic rigor.
On January 13, 2026 AT 16:30
James Castner
Imagine your kidneys as a city’s water filtration plant. If it’s still pumping out clean water, you assume it’s fine-until one day, the sewage starts leaking into the reservoir. No alarms. No warnings. Just a slow, silent contamination. That’s stage 1 CKD. And here’s the truth: most people don’t realize they’re living in a city with a broken filter until the whole system collapses. But we can fix it-if we’re willing to look beyond the surface numbers. The two-test rule isn’t just clinical protocol-it’s a moral imperative. We owe it to every silent, failing organ to see them clearly.
On January 15, 2026 AT 13:22
Adam Rivera
My uncle was diagnosed at stage 3b after a routine check-up. He didn’t even know he had diabetes. But they caught it early because his doctor ordered both tests. He’s still walking, still cooking, still teasing his grandkids. It’s not magic-it’s just paying attention. You don’t need a fancy lab. You just need someone who knows what to ask for.
On January 15, 2026 AT 19:38
Rosalee Vanness
Let me tell you something-your kidneys don’t throw parties when they’re failing. They don’t send you text messages saying, ‘Hey, I’m about to quit.’ They just… fade. Like a candle in a windless room. And when you finally notice? It’s too late to relight it. But if you catch it early? You can still turn the dial back. A little protein in your pee? That’s your body whispering. Listen. Don’t wait for it to scream. Get the uACR. Get the eGFR. Do it now. For yourself. For the people who love you. Don’t let silence be your enemy.
On January 16, 2026 AT 16:25
lucy cooke
Oh, this is just beautiful. Another soulless algorithm masquerading as medicine. We’ve turned human bodies into spreadsheets. eGFR? uACR? What’s next? A QR code on your kidney? We used to listen. Now we just scan. And when the numbers are ‘normal,’ we pretend the silence means peace. But silence isn’t peace-it’s the calm before the storm. And the storm? It’s coming. For all of us.
On January 17, 2026 AT 09:47
Trevor Davis
I used to be a nurse. I’ve seen people come in with creatinine at 1.2, all happy, thinking they’re fine. Then we do the uACR-and boom. 400 mg/g. They’re crying before they even understand why. This isn’t about tests. It’s about fear. People don’t want to know. But knowing? That’s the only thing that saves you.
On January 18, 2026 AT 01:53
John Tran
ok so like… i was just at the dr and they did the creatinine thing and said im fine. but now im reading this and im like… wait… did they skip the other test?? i think they did. i’m 42, diabetic, kinda fat, but my creatinine was 0.9 so they said ‘you’re good’. now im sweating. i need to go back. like tomorrow. this is scary. someone please tell me i’m not the only one who got fooled.
On January 18, 2026 AT 03:29
Jesse Ibarra
Of course you need both tests. Anyone who doesn’t know this is either a quack or a liar. And if your doctor is skipping uACR, they’re not just negligent-they’re dangerous. This isn’t debate. It’s malpractice. And if you’re reading this and you’re over 40? Go get both tests today. Don’t wait for a ‘recommendation.’ Demand it. Your life isn’t a suggestion.
On January 18, 2026 AT 20:58
laura Drever
Yeah right. Another article from a guy who thinks numbers fix everything. Kidneys aren’t math problems. People are. You think a test tells you if someone eats too much salt? Or drinks soda all day? Or doesn’t sleep? Nah. It just gives you a number to feel good about. Meanwhile, the real problem? Lifestyle. But that’s too hard to fix. So we test instead.
On January 20, 2026 AT 00:20
Randall Little
So let me get this straight: you’re telling me that for decades, doctors ignored protein in urine because they were too lazy to run a second test? And now we’re acting like this is some revolutionary breakthrough? The real scandal isn’t that CKD is missed-it’s that we’re still surprised it’s missed. Wake up. This isn’t science. It’s systemic laziness dressed up in white coats.
On January 21, 2026 AT 23:20
Pankaj Singh
What nonsense. In India, we don’t have money for two tests. We have one test. And if it’s normal, we move on. You think your fancy American protocols save lives? They just make the rich feel safe. The poor? They die quietly. No uACR. No eGFR. Just silence. And you write articles like this like it’s a moral victory. It’s not. It’s privilege.
On January 23, 2026 AT 13:55
Robin Williams
bro. i just found out my dad has stage 2. he’s 58. he’s been drinking diet coke like water and eating chips every night. we thought he was fine. we didn’t even know this uACR thing existed. now i’m gonna make him go get tested. i’m gonna print this out and tape it to his fridge. if this saves one life, it’s worth it.
On January 23, 2026 AT 21:46
Scottie Baker
My sister died at 41. Stage 5. They didn’t catch it till she was in the ER, coughing blood. They said her creatinine was ‘normal.’ She had no symptoms. Just… gone. If they’d done the second test… she’d be here. I hate that I’m the one who has to tell people this. But I will. Every. Single. Time.
On January 25, 2026 AT 17:58