When you're stuck in a loop of negative thoughts-worrying about everything, blaming yourself, dreading social situations-it's not just being "overly sensitive." It's your brain learning to think in ways that hurt you. That’s where cognitive behavioral therapy comes in. Unlike talk therapies that dig deep into childhood, CBT is practical, focused, and built on decades of hard science. It doesn’t promise quick fixes, but it does give you tools you can use right away to feel better.
What Exactly Is Cognitive Behavioral Therapy?
Cognitive behavioral therapy, or CBT, is a type of psychological treatment that looks at how your thoughts, feelings, and behaviors connect. It’s not about rehashing your past. It’s about understanding what’s happening right now and changing it.
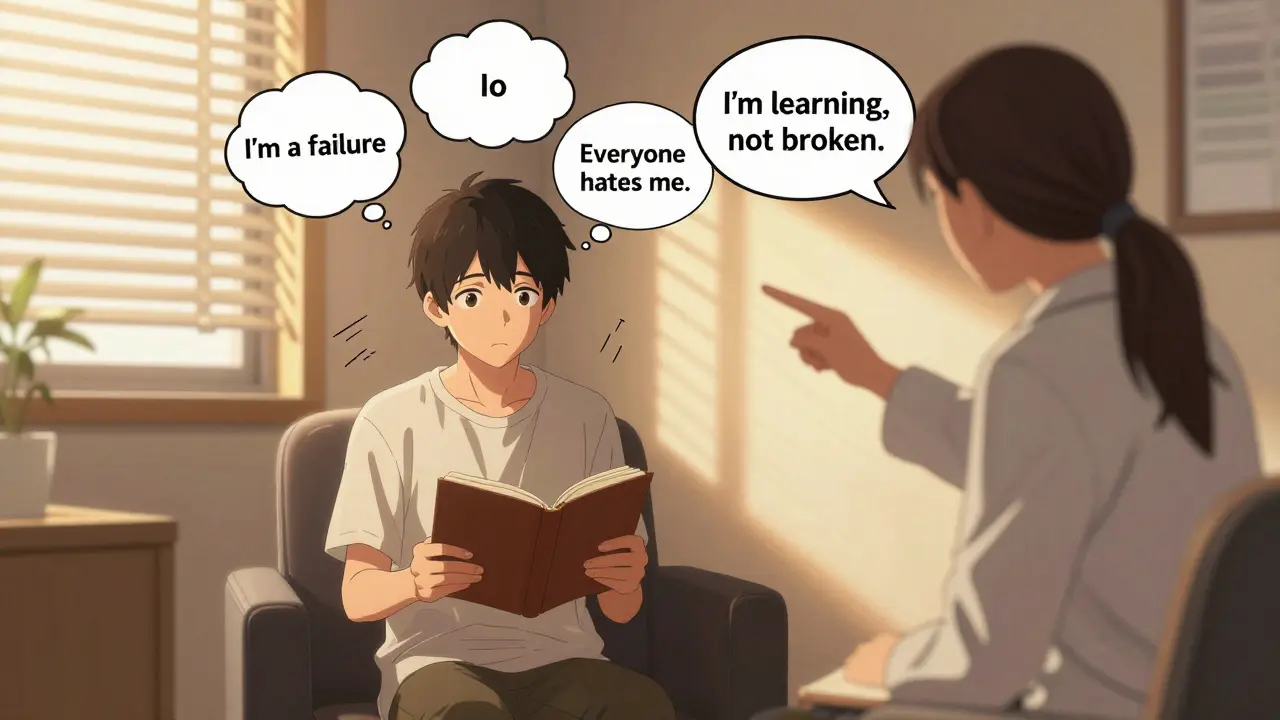
It was developed in the 1960s by psychiatrist Aaron T. Beck. He noticed that people with depression weren’t just sad-they were thinking in distorted ways. "I’m a failure," "No one cares," "The future is hopeless." These weren’t just moods. They were beliefs that kept the sadness going. Beck realized: if you change the thinking, you can change the feeling.
CBT combines two parts:
- Cognitive - how you think
- Behavioral - what you do
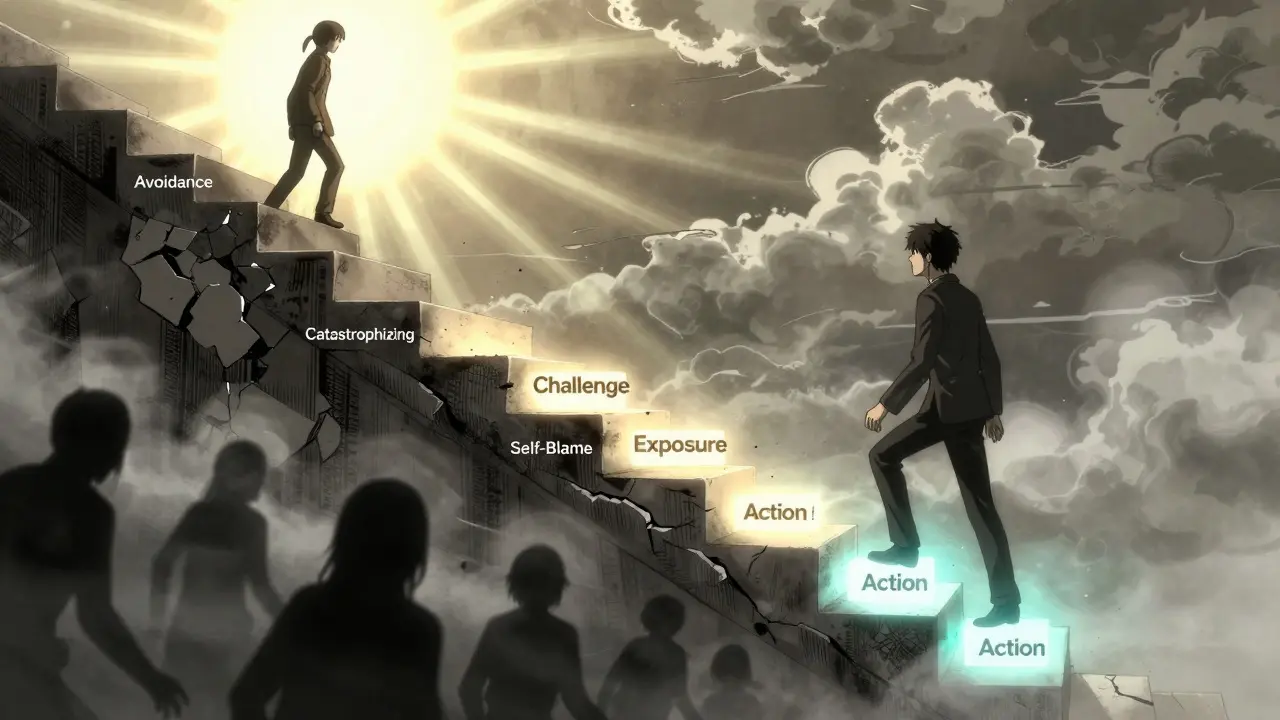
It’s not vague advice like "just be positive." It’s structured. You learn to spot automatic negative thoughts, test them against reality, and replace them with something more balanced. Then you take action-do the thing you’ve been avoiding, face the fear, try something new.
Why Is CBT Called "Evidence-Based"?
CBT isn’t popular because it sounds nice. It’s popular because it works-and we have the data to prove it.
Over 2,000 randomized controlled trials have tested CBT since the 1970s. That’s more than any other form of therapy. The National Institute for Health and Care Excellence (NICE) in the UK has listed CBT as a first-line treatment for depression, anxiety, PTSD, OCD, and eating disorders since 2004. The American Psychological Association calls it the "gold standard."
Here’s what the numbers show:
- For anxiety disorders, 60-80% of people see major improvement after 12-16 sessions.
- For major depression, CBT has a 52% remission rate at 12 months-better than antidepressants alone, and with far lower relapse rates (24% vs. 52%).
- For OCD, Exposure and Response Prevention (a type of CBT) leads to full symptom remission in many cases after 18 sessions.
It’s not just lab results. In NHS England’s 2023 survey of 15,000 patients, 68% reported significant symptom reduction. On Psychology Today, 87% of users rated CBT as "very" or "extremely" effective for anxiety.
How Does CBT Actually Work?
CBT isn’t magic. It’s a toolkit. Therapists use eight core techniques, all backed by research:
- Identifying cognitive distortions - like catastrophizing ("I’ll never get over this") or mind reading ("They all think I’m weird").
- Challenging automatic thoughts - asking: "What’s the evidence for this? What’s another way to see this?"
- Modifying core beliefs - digging deeper than surface thoughts. "I’m unlovable" might be the root behind every failed relationship.
- Behavioral activation - getting moving again, even when you don’t feel like it. Depression drains energy; action rebuilds it.
- Exposure techniques - slowly facing fears. Not all at once. Step by step. Like talking to one person, then two, then a group.
- Skills training - learning how to communicate, manage stress, say no, or sleep better.
- Relapse prevention - planning what to do if symptoms come back.
- Homework - writing thought records, trying new behaviors, tracking mood. This is where real change happens.
Most sessions last 45-60 minutes and happen weekly. A full course usually takes 5 to 20 sessions. That’s much shorter than traditional therapy, which can last years.
What Conditions Does CBT Help With?
CBT isn’t a one-size-fits-all. It’s been adapted for dozens of conditions:
- Anxiety disorders - social anxiety, panic disorder, generalized anxiety
- Depression - especially mild to moderate cases
- PTSD - trauma-focused CBT helps process memories without getting stuck
- OCD - Exposure and Response Prevention is the most effective treatment
- Eating disorders - helps break the cycle of restriction, bingeing, guilt
- Insomnia - CBT-I (Cognitive Behavioral Therapy for Insomnia) is recommended before sleeping pills
- Chronic pain - teaches how to manage pain without letting it control your life
- Substance use - helps identify triggers and build coping skills
The NHS and WHO include CBT in their official guidelines for all of these. It’s not experimental. It’s standard care.
How Does CBT Compare to Other Treatments?
People often wonder: should I try CBT, medication, or both?
Here’s how CBT stacks up:
| Treatment | Effectiveness for Depression | Relapse Rate (12 Months) | Duration |
|---|---|---|---|
| CBT | 52% remission rate | 24% | 12-16 sessions |
| Antidepressants | 47% remission rate | 52% | Ongoing |
| CBT + Antidepressants | 60% remission rate | 18% | 12-16 sessions + medication |
| 12-Step Programs (for addiction) | 25-35% abstinence | N/A | Long-term |
| CBT for Addiction | 40-60% abstinence | N/A | 12-20 sessions |
For anxiety, CBT’s effect size is 0.77-1.14. Other therapies hover around 0.58-0.89. That’s a meaningful difference.
But CBT isn’t perfect. For severe trauma or borderline personality disorder, Dialectical Behavior Therapy (DBT) works better. For young children with behavioral issues, Parent-Child Interaction Therapy has shown 25% better results.
Who Might Not Benefit from CBT?
CBT requires effort. You have to show up, do the homework, and sit with discomfort. That’s hard.
People who struggle with:
- Severe cognitive impairment - like advanced dementia or intellectual disability
- Acute psychosis - where thoughts are detached from reality
- Extreme emotional overwhelm - who can’t focus enough to do thought records
May need other approaches first. CBT isn’t for everyone-but it’s the best starting point for most.
What Do People Really Say About CBT?
Real stories matter more than stats.
One person on Reddit said: "I did a thought record for three weeks. I realized I was assuming everyone thought I was boring. Turns out, no one even noticed. That changed everything."
Another shared: "I had panic attacks 15 times a week. My therapist had me go to the grocery store alone for five minutes. Then ten. Then 20. Within six weeks, I was shopping without shaking."
But it’s not all easy. In 32% of negative reviews, people say homework felt overwhelming. In 27%, exposure exercises were too scary at first.
That’s normal. CBT isn’t supposed to feel comfortable. It’s supposed to stretch you. The discomfort is the price of change.

How Do You Get Started?
In the UK, you can get CBT through the NHS. Ask your GP for a referral to an IAPT service (Improving Access to Psychological Therapies). Wait times vary, but it’s free.
If you’re paying privately, look for therapists certified by the British Association for Behavioural and Cognitive Psychotherapies (BABCP). They’ve completed 120-180 hours of training and supervised cases.
You can also try digital CBT. Apps like Woebot (FDA-cleared) offer guided sessions. But studies show in-person CBT is 22% more effective. Use apps as a supplement, not a replacement.
Free resources exist too. The National Alliance on Mental Illness (NAMI) offers downloadable CBT workbooks. The Beck Institute has free videos and exercises online.
What’s Next for CBT?
CBT isn’t stuck in the past. New versions are emerging:
- Third-wave CBT - includes mindfulness and acceptance. Acceptance and Commitment Therapy (ACT) works better for chronic pain.
- AI-assisted CBT - tools that analyze your thought records in real time, giving instant feedback.
- Personalized CBT - future versions may match your brain activity, genetics, or stress response to the best technique.
But the core stays the same: thoughts affect feelings. Feelings affect actions. Change one, and you change the others.
Is CBT Worth It?
If you’re tired of feeling stuck, anxious, or down-and you’re ready to do the work-then yes. CBT is the most proven, practical, and powerful psychological treatment we have.
You don’t need to understand neuroscience. You don’t need to relive your childhood. You just need to ask: "Is this thought helping me?" and then try something different.
It’s not a miracle. But it’s real. And for millions, it’s changed everything.
Can CBT help with anxiety even if I’ve tried medication before?
Yes. Many people find CBT works better than medication alone, especially for long-term results. While antidepressants can reduce symptoms quickly, they don’t teach you how to manage anxiety when it comes back. CBT gives you skills to handle triggers, reduce avoidance, and reframe thoughts-so anxiety doesn’t control you. Studies show combining CBT with medication leads to the highest success rates and lowest relapse.
How long does it take to see results with CBT?
Most people notice small improvements within 4-6 sessions. For anxiety or depression, significant change usually happens between 8 and 12 weeks. The key is consistency. Doing your homework-even just 15 minutes a day-makes the difference. It’s not about how fast you feel better, but how deeply you learn to manage your thoughts and behaviors.
Do I need a therapist for CBT, or can I do it on my own?
You can start with self-help books or apps, and many people benefit. But working with a trained therapist increases success by 20-30%. Therapists help you spot blind spots in your thinking, adjust techniques if something isn’t working, and provide accountability. For moderate to severe symptoms, professional guidance is strongly recommended.
Is CBT only for depression and anxiety?
No. CBT is used for over a dozen conditions, including OCD, PTSD, insomnia, chronic pain, eating disorders, substance use, and even anger management. The core principles-identifying unhelpful thoughts and changing behaviors-apply to almost any issue where emotions and actions are stuck in a negative cycle.
What if I don’t believe in "thinking" my way out of problems?
That’s common. Many people think CBT is too "mental"-like you’re just talking to yourself. But CBT isn’t about positive thinking. It’s about testing thoughts like hypotheses. Is it true that "I’ll never get better"? What’s the evidence? What’s the opposite? You’re not forcing optimism-you’re checking reality. And then you act. Even if you don’t believe it at first, doing the behavior anyway (like going to a party, or getting out of bed) often changes how you feel.
Are CBT sessions covered by insurance in the UK?
Yes. Through the NHS, CBT is fully covered under the IAPT program. If you’re seeing a private therapist, many private health insurance plans in the UK cover CBT if the therapist is accredited by BABCP or BPS. Always check your policy, but CBT is one of the most commonly reimbursed therapies because of its proven effectiveness.

Comments
Darren McGuff
I was skeptical at first, but after 14 sessions of CBT for social anxiety, I went from avoiding parties to hosting them. Not because I suddenly became extroverted, but because I stopped believing everyone was judging me. Turns out, most people are too busy worrying about themselves to notice if you spilled your drink.
Homework felt like a chore at first-writing down thoughts like some kind of emotional diary-but it worked. I started catching myself before I spiraled. That’s the magic: it’s not about fixing you. It’s about teaching you how to observe yourself.
CBT didn’t make me happy. It made me less afraid of being unhappy. And that’s worth every minute.
On January 8, 2026 AT 20:18
Alicia Hasö
For anyone reading this and thinking, ‘I’m too broken for this’-you’re not. CBT isn’t for the ‘well-adjusted.’ It’s for the exhausted. The ones who lie awake wondering why they said that one thing five years ago. The ones who cancel plans because their brain screams, ‘They’ll hate you.’
You don’t need to believe in it to benefit from it. Just show up. Do the worksheet. Say the sentence out loud. Even if you feel ridiculous. That’s the point-you’re rewiring a brain that learned to lie to you. And you deserve to unlearn it.
On January 9, 2026 AT 00:52
Ashley Kronenwetter
While CBT has strong empirical support, it is important to acknowledge that not all populations respond equally. Cultural factors, linguistic barriers, and socioeconomic constraints can significantly affect therapeutic outcomes. Standardized CBT protocols, developed primarily in Western clinical contexts, may not fully account for collectivist or non-individualistic cognitive frameworks. A one-size-fits-all approach risks unintentional pathologizing of culturally normative thought patterns.
On January 10, 2026 AT 15:46
Aron Veldhuizen
Let’s be real-CBT is just cognitive suppression dressed up in clinical jargon. You’re not changing thoughts, you’re just teaching people to censor them. What about the root causes? Trauma? Capitalist alienation? The fact that the world is objectively terrifying?
They tell you to ‘challenge your negative thoughts’-but what if your thoughts are accurate? What if everyone really does think you’re weird? What if your boss is a narcissist and your rent is unaffordable? CBT doesn’t fix systems. It just makes you better at pretending the system isn’t crushing you.
It’s psychological gaslighting with a certificate.
On January 11, 2026 AT 02:55
Heather Wilson
68% improvement? That’s a nice number, but let’s look at attrition. Most people drop out before session 6. The homework is too much. The exposure is too scary. The whole thing feels like a productivity hack for emotional pain. And don’t get me started on the ‘gold standard’ nonsense-every therapy has flaws. Why is CBT the only one treated like gospel?
Also, the study cited from NHS England? They self-reported. No control group. No blinding. Hardly rigorous. And why is nobody talking about the fact that 32% of people found the homework overwhelming? That’s not a feature-that’s a design flaw.
On January 12, 2026 AT 16:50
Micheal Murdoch
I’ve sat with people in therapy rooms, in ER waiting areas, in college counseling centers-people who’ve been told they’re ‘just anxious’ or ‘just depressed’ for years. CBT is the first thing that ever made them feel seen, not fixed.
It’s not about being positive. It’s about being honest-with yourself, with your thoughts, with your fear. I’ve seen people who couldn’t leave their house for six months learn to take the bus to the corner store. Not because they were magically cured. But because they learned to ask: ‘Is this thought helping me survive-or just hurting me?’
That’s not magic. That’s courage. And it’s available to anyone willing to sit with the discomfort.
You don’t need to believe in CBT. You just need to try one thought record. One day. One small step. That’s all it takes to start.
On January 14, 2026 AT 14:17
Jeffrey Hu
Everyone’s acting like CBT is the only thing that works. Have you heard of schema therapy? Or EMDR? Or ACT? Or even psychodynamic therapy? CBT’s popularity is just a product of insurance reimbursement models and corporate wellness trends. It’s cheap, short, and measurable-perfect for bureaucracies, not human suffering.
Also, the ‘52% remission rate’? That’s barely better than placebo in some meta-analyses. And relapse rates? You’re comparing it to meds, but not to other therapies. CBT’s not the god-tier treatment-it’s the default because it’s the easiest to train people in.
On January 16, 2026 AT 07:55
Drew Pearlman
I know this sounds cheesy, but I’m alive today because of CBT.
Five years ago, I was on the edge. Every morning felt like climbing a mountain in concrete boots. My therapist didn’t tell me to cheer up. She gave me a notebook and said, ‘Write down the thought right before you feel like giving up.’
My first entry: ‘I’m a burden.’
Second: ‘No one would miss me.’
Third: ‘I’m tired of pretending.’
Then we asked: ‘What’s the evidence?’ I wrote: ‘I haven’t told anyone how I feel.’
That was the turning point. Not because I suddenly felt better. But because I realized-I hadn’t even given anyone a chance to care.
CBT didn’t fix me. It gave me a flashlight in the dark. And sometimes, that’s enough.
On January 18, 2026 AT 03:35
Chris Kauwe
Let’s not pretend this is some revolutionary Western innovation. Ancient Stoics were doing CBT 2,000 years ago. Marcus Aurelius wrote thought records before it was cool. Epictetus said, ‘It’s not events that disturb us, but our opinions about them.’ That’s CBT 101.
Now we’ve packaged it in a 12-session NHS program and sold it like a tech startup. We’ve stripped away the philosophy, turned it into a checklist, and called it ‘evidence-based.’
Don’t get me wrong-it works. But it’s not new. It’s just been rebranded for the attention economy.
On January 18, 2026 AT 18:37
Meghan Hammack
My mom had panic attacks for 12 years. She tried meds, acupuncture, yoga, crystals-nothing worked. Then she did CBT. Not because she believed in it. Because her doctor said, ‘Try this for 8 weeks.’
She hated the homework. Said it felt like school. But she did it anyway. One day, she walked into a grocery store alone. Didn’t panic. Didn’t run. Just… bought milk.
That was it. No big speech. No epiphany. Just milk. And then she did it again. And again.
It wasn’t magic. It was muscle. And now? She travels alone. Talks to strangers. Sleeps through the night.
You don’t need to understand psychology. You just need to show up. Even when it sucks.
On January 19, 2026 AT 01:04
RAJAT KD
CBT saved my life. Done.
On January 19, 2026 AT 03:16
Matthew Maxwell
It’s alarming how casually people treat CBT as a universal solution. The data is cherry-picked. The studies are industry-funded. The patients who drop out are ignored. And the people who fail? They’re told they ‘didn’t try hard enough.’
This isn’t therapy. It’s behavioral conditioning for a society that wants quick fixes for systemic problems. If you’re depressed because you’re working 60 hours a week for $15 an hour, CBT won’t fix your wage. It’ll just make you feel guilty for not being ‘positive’ enough.
Stop glorifying psychological band-aids.
On January 19, 2026 AT 20:40
Lindsey Wellmann
OMG I CRY EVERY TIME I READ THIS 😭💖
CBT literally gave me back my life 🙏✨ I went from hiding in my room for 3 months to giving a TEDx talk on anxiety (yes, really) and I’m not even joking!!
My therapist was a goddess 🌟 and the homework? I did it with my cat on my lap 🐱☕️
If you’re reading this and thinking ‘I can’t’-you already are. Just start. One thought. One breath. One step. I believe in you 💕🌈
On January 20, 2026 AT 11:01