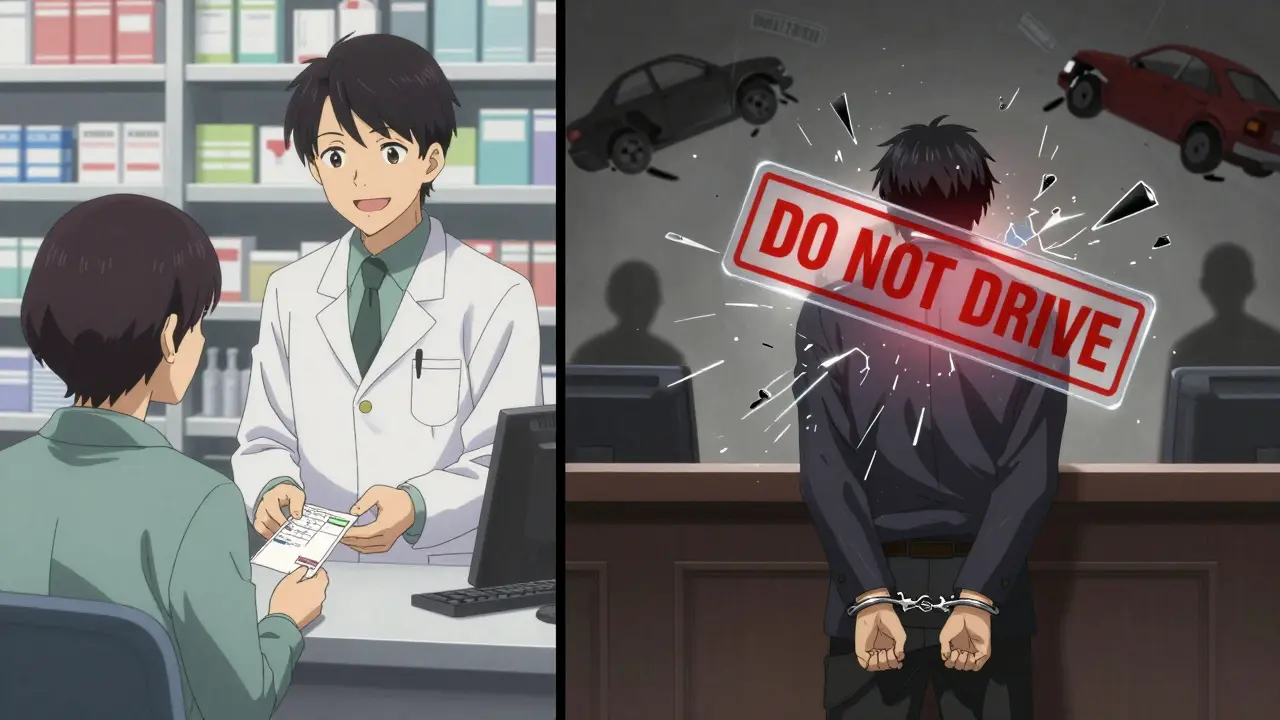
Driving while taking opioids isn't just risky-it's illegal in every U.S. state and Canadian province. Even if your doctor prescribed the medication, and you're taking it exactly as directed, you could still be charged with a DUI. Many people don’t realize this until they’re pulled over, fail a sobriety test, or get arrested after a minor fender bender. The truth is, opioids don’t just dull pain-they dull your ability to drive safely.
How Opioids Affect Your Driving Skills
Opioids like oxycodone, hydrocodone, morphine, and fentanyl slow down your central nervous system. That’s why they work for pain-but it’s also why they make driving dangerous. The National Institute on Drug Abuse (NIDA) says these drugs cause drowsiness, dizziness, and impaired thinking. Simple tasks like judging distance, reacting to a sudden stop, or staying in your lane become harder. Studies show that driving under the influence of opioids can double your risk of a crash.
Unlike alcohol, where blood levels correlate closely with impairment, opioids don’t have a clear “legal limit.” One person might feel fine after 5 mg of oxycodone, while another could be dangerously impaired on the same dose. This unpredictability is why even prescribed use doesn’t guarantee safety behind the wheel.
Legal Consequences Are Real-and Harsh
In 16 U.S. states, any detectable amount of an opioid in your system while driving is enough to get you charged with a DUI. These are called “zero-tolerance” laws. Five other states have “per se” laws, meaning if you have certain levels of opioids in your blood, you’re automatically considered impaired-even if you’re not acting drunk.
Canada treats opioid-impaired driving the same as alcohol-impaired driving under its Criminal Code. Fines, license suspension, and jail time apply regardless of whether the drug was prescribed.
Some states offer narrow defenses. Utah allows you to argue the opioid was prescribed by a doctor. Georgia lets drivers under 21 claim they were using it “therapeutically.” Wisconsin requires you to prove by a preponderance of evidence that you had a valid prescription. But these exceptions are rare. In most places, having a prescription doesn’t protect you from arrest.
Why Law Enforcement Struggles to Detect Opioid Impairment
Police use Standardized Field Sobriety Tests (SFST)-walking heel-to-toe, standing on one leg, following a pen with your eyes. But these tests were designed for alcohol. Opioid impairment looks different. You might not smell like liquor, stumble, or slur your words. Instead, you could appear sleepy, slow to respond, or confused.
Officers trained in the Drug Evaluation and Classification (DEC) program can spot signs like pinpoint pupils, slow reaction times, and unusual posture. But not every officer has this training. That’s why many opioid-impaired drivers aren’t caught until after a crash.
Technology is catching up. In 2023, the FDA approved the Dräger DrugTest 5000, a roadside device that detects fentanyl and other synthetic opioids in oral fluid. Forty-seven states now use these devices-up from just 32 in 2020. But they’re still not foolproof. Labs can take days to confirm results, and the presence of a drug doesn’t always prove impairment.

What People Don’t Realize About Prescription Opioids
A 2022 survey by the Pain News Network found that 63% of chronic pain patients didn’t know driving on prescribed opioids could lead to a DUI. One Reddit user, u/PainPatient88, wrote: “My doctor said it was fine to drive on 5mg oxycodone twice daily. I failed a field sobriety test after my prescription was filled.” Another user, u/RecoveryJourney, lost his license for six months and paid $12,000 in legal fees-even though he took his meds exactly as prescribed.
Pharmacists often don’t warn patients either. A Drugs.com survey showed 78% of opioid users reported warnings about driving on the label-but many said their pharmacist told them it was “fine.” That’s dangerous misinformation. The FDA has required all opioid packaging to include “Do Not Drive” warnings since 2020, but patients still aren’t getting the message.
When Is It Safe to Drive After Taking Opioids?
There’s no universal answer. It depends on the drug, the dose, your metabolism, and whether you’re taking other medications.
For immediate-release opioids like hydrocodone or oxycodone, the Mayo Clinic recommends waiting at least 3-4 hours after taking a dose. For extended-release versions like OxyContin or MS Contin, wait 6-8 hours. But even then, you might still feel drowsy. The safest rule? Don’t drive the first few days after starting a new opioid, after a dose increase, or if you’re mixing it with alcohol, benzodiazepines, or sleep aids.
Some people think they’re “used to” the medication and can drive safely. That’s a myth. Tolerance to pain relief doesn’t mean tolerance to impairment. Your brain still processes information slower.
What You Should Do Instead
Plan ahead. If you’re prescribed opioids, ask your doctor: “Will this make me too drowsy to drive?” Don’t assume it’s safe just because it’s legal. Ask your pharmacist for written instructions. Check the medication guide that comes with your prescription-it’s required by law to include driving warnings.
Use alternatives: Take public transit, call a ride-share, or ask a friend or family member to drive you. The California Office of Traffic Safety says: “Plan ahead for a sober driver if you plan to use an impairing drug.” It’s not an option-it’s a necessity.
Wear your seatbelt. Even if you’re not the one impaired, you’re still at risk from other opioid-drivers. In 2018, 42% of drivers killed in crashes tested positive for drugs-legal or illegal.
What’s Changing in 2025?
The federal government is stepping up. In 2023, the National Highway Traffic Safety Administration launched a $9.2 million initiative to train 5,000 new Drug Recognition Experts by 2025. States are rushing to update laws-seven more are considering per se limits for opioids in 2024.
The DEA reports a 262% increase in fentanyl-related impaired driving cases between 2020 and 2023. Fentanyl is 50-100 times stronger than morphine. Just a tiny amount can knock you out. That’s why detection tools and laws are playing catch-up-and why the risk is growing faster than ever.
Employers are reacting too. UPS now requires mandatory medical reviews for any employee prescribed opioids. Since 2021, they’ve seen a 37% drop in medication-related incidents. If a delivery company can enforce this, so can you.
Final Warning: This Isn’t a Risk Worth Taking
Driving on opioids isn’t a gray area. It’s a clear, dangerous line. You don’t need to be “high” to be impaired. You don’t need to be using street drugs. Even a single prescribed pill can make you a danger to yourself and others.
There’s no excuse for not planning ahead. No doctor’s note, no pharmacy reassurance, no personal experience overrides the science. Your brain doesn’t work the same. Your reflexes are slower. Your judgment is clouded.
If you’re on opioids, drive only if you’re 100% certain you’re not impaired. And if you’re not sure? Don’t risk it. Call someone. Wait. Take a bus. The consequences aren’t just legal-they’re life-altering.
Support is available. The Substance Abuse and Mental Health Services Administration (SAMHSA) helpline-1-800-662-4357-received over 12,000 calls in 2022 about medication-related driving risks. You’re not alone. But you are responsible.

