More than 90% of prescriptions in the U.S. are filled with generic drugs. They cost 80-85% less than brand-name versions and are just as safe and effective. Yet, many patients still hesitate to take them. Why? It’s not because the science is weak-it’s because the message hasn’t been delivered well.
Why Patients Doubt Generic Medications
Patients aren’t being irrational. They’ve heard stories. Maybe a relative said their generic version of Sertraline made them feel worse. Or they saw a different-looking pill and assumed it was inferior. Some think, "If it’s cheaper, it must be less good." That’s not how the FDA works. The FDA requires generics to match brand-name drugs in active ingredients, dosage, strength, route of administration, and performance. They must show bioequivalence-meaning the body absorbs the drug at the same rate and to the same extent. The acceptable range? 80% to 125% of the brand’s absorption. That’s tight. That’s science. But perception doesn’t follow data. A 2024 study in PLOS ONE found that nearly 40% of Americans still believe generics have more side effects. Among patients with low health literacy, over half thought generics were less effective or less safe. Older adults, employed people, and those with private insurance were more confident. Non-white patients and those on Medicaid were significantly less so. This isn’t about intelligence. It’s about trust, communication, and past experiences.The Role of the Pharmacist
Pharmacists are the most trusted source of drug information after doctors. Yet, too often, they’re rushed. A patient walks up, gets a new bottle, and hears, "It’s the same thing, just cheaper." That’s not education. That’s dismissal. Research shows that when a pharmacist takes just 2-3 minutes to explain why the switch is safe, patient comfort jumps from 63% to 85%. That’s not magic. That’s clarity. A good conversation includes:- "This is the same medicine your doctor prescribed, just made by a different company."
- "The FDA checks it just as closely as the brand name."
- "It’s been used by millions of people with the same results."
- "If you’ve had side effects before, let’s talk about what to watch for."
Doctors Need to Speak Up Too
Doctors hold the most influence. If a physician says, "I’m prescribing this generic because it works just as well and saves you money," patients believe it. If they don’t mention it at all, patients assume the doctor doesn’t trust it. A 2023 FDA publication highlighted this clearly: "Taking time to talk with patients about switching from brand-name to generic drugs can increase their confidence." That’s not a suggestion. That’s a requirement for good care. In Greece, 70% of patients accepted generics when their doctor recommended them. In the U.S., the number is even higher-but only when communication happens. The key isn’t just prescribing generics. It’s intentionally discussing them.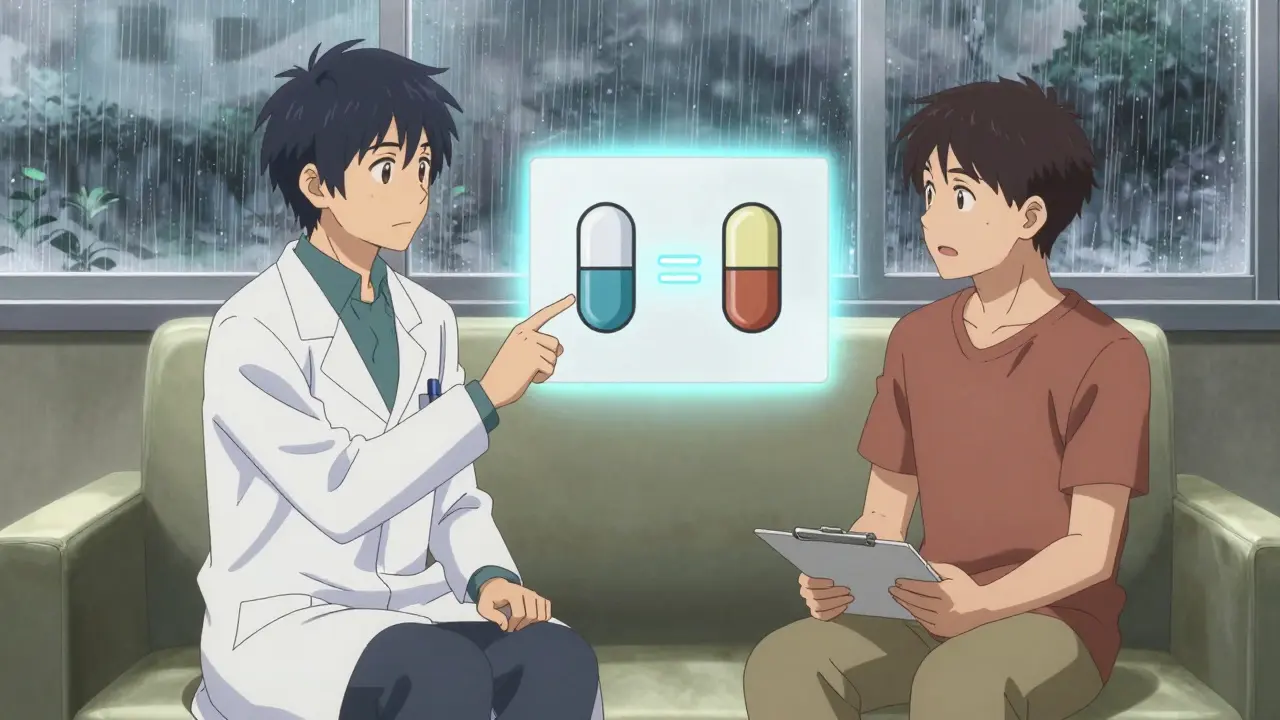
What Patients Are Really Afraid Of
Fear isn’t abstract. It’s specific:- 29.5% worry about new or worse side effects
- 25.7% just don’t want to change what’s working
- 24.1% doubt the medicine will work as well
- 20.8% say they’d rather pay more for peace of mind
What Works: Real Strategies from Real Studies
Here’s what the research says actually moves the needle:- Use plain language. Don’t say "bioequivalence." Say, "Your body gets the same amount of medicine from this pill as the brand name."
- Provide written materials. 62% of patients found pharmacy pamphlets "somewhat helpful." Make them better. Use pictures. Use real patient stories. Include the FDA’s official statement: "Generic drugs have the same quality, strength, purity, and stability as brand-name drugs."
- Train staff. Pharmacists and nurses need to know how to answer common myths: "No, generics don’t use lower-quality ingredients. They’re made in the same type of factories, under the same rules."
- Ask for consent. Patients want to be part of the decision. Don’t substitute without telling them. Say, "I’m going to give you the generic version unless you’d prefer to stick with the brand."
- Follow up. A quick call or message a week after switching: "How are you feeling? Any changes?" That simple check-in reduces anxiety and builds trust.
What Doesn’t Work
Avoid these common mistakes:- Assuming patients know what "generic" means. Many think it means "cheap copy." It doesn’t.
- Blaming patients for being "uninformed." The system failed them first.
- Using jargon. "Pharmaceutical equivalence" means nothing to someone trying to pay rent.
- Letting insurance dictate the conversation. "Your plan requires it" isn’t a reason-it’s a transaction.

When Generics Are Tricky
Some drugs are harder to switch. Complex delivery systems-like inhalers, patches, or injectables-can feel different even when they’re identical in active ingredients. A patient might say, "This inhaler doesn’t feel the same." That’s not always about the medicine. It’s about the device. In these cases, hands-on instruction matters. Show the patient how to use it. Let them practice. Compare the feel side by side. That’s not extra work. It’s essential care.Why This Matters Beyond Cost
Saving money is important. But the bigger win is adherence. When patients trust their meds, they take them. When they don’t, they skip doses, stop early, or switch back to more expensive options. The Congressional Budget Office estimates generics will save the U.S. healthcare system $1.7 trillion over the next decade. But that only happens if people keep taking them. And they’ll only keep taking them if they believe in them.The Bottom Line
Generic drugs aren’t a compromise. They’re the standard. They’re proven. They’re safe. But belief doesn’t come from a label. It comes from a conversation. If you’re a clinician, pharmacist, or even a caregiver-you have the power to change how patients see generics. Not with brochures. Not with ads. With words. With time. With honesty. Start tomorrow. Ask one patient: "Have you ever had concerns about switching to a generic?" Listen. Then explain. That’s all it takes.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning your body absorbs them at the same rate and to the same extent. Studies show no meaningful difference in effectiveness or safety between generics and brand-name drugs in real-world use.
Why do some people say their generic medicine doesn’t work the same?
Sometimes, it’s about expectations. If a patient has been on a brand-name drug for years, switching to a generic with a different color or shape can feel like a change-even when the medicine is identical. Rarely, differences in inactive ingredients (like fillers or dyes) may cause minor reactions in sensitive individuals. But these are exceptions, not the rule. If side effects appear after switching, talk to your provider. It’s not proof the generic is inferior-it’s a sign to investigate further.
Can pharmacists substitute generics without asking me?
In 18 U.S. states, pharmacists can substitute generics without notifying the prescriber. But they’re still required to inform you. Ethical practice means always telling patients about the switch, even if the law doesn’t require it. You have the right to know what you’re taking-and to say no if you prefer the brand.
Why do generics cost so much less if they’re the same?
Brand-name drugs include the cost of research, development, marketing, and patent protection-often billions of dollars. Generics skip all that. They’re made after the patent expires, using the same formula. No need to spend on ads or clinical trials. That’s why they’re cheaper-not because they’re lower quality.
What should I do if I’m worried about switching to a generic?
Talk to your pharmacist or doctor. Ask them to explain how the generic is tested and approved. Request written information from the FDA or your pharmacy. If you’re still unsure, ask to stay on the brand for now. Your comfort matters. But know this: millions of people switch safely every day. The science is solid. The fear is often about the unknown.

Comments
Katie Schoen
So let me get this straight - we’re spending billions on brand-name drugs just because people think the pill looks prettier? I’ve taken generics for my blood pressure for 7 years. Same results. Same side effects. Same nothing. The only thing that changed? My wallet stopped crying.
On January 6, 2026 AT 03:31
Pavan Vora
My cousin in Delhi, he took generic metformin... then he got dizzy. He thought it was the medicine. Turned out, he skipped breakfast. But now he refuses all generics. Said, 'If it's cheap, it's for poor people.' I told him, 'Bhai, even the rich take generics - they just don't admit it.' He still won't believe. Culture, man. It's deeper than science.
On January 8, 2026 AT 00:33
Indra Triawan
It’s not about the pills. It’s about control. When you’re sick, you want to cling to something familiar - even if it’s a lie. The brand name feels like a promise. The generic? Just a receipt. We don’t trust systems. We trust stories. And nobody told us the story of the generic. They just handed it over like a coupon.
On January 9, 2026 AT 23:56
Wesley Pereira
Pharmacies are just pharmacy *factories*. They don’t care if you live or die, as long as the script clears. I got switched to a generic levothyroxine and my TSH went nuclear. Took me 3 months to get back on brand. Turns out, the generic had a different filler that messed with absorption. FDA’s 80-125% range? That’s a fucking loophole. Not all generics are created equal. And yeah, I’m mad.
On January 10, 2026 AT 11:24
Dana Termini
I’m a nurse. I’ve seen patients cry because they think switching to a generic means their doctor gave up on them. That’s not about the drug - it’s about feeling abandoned. The moment I started saying, ‘Your doctor chose this because they care enough to help you save money without sacrificing care,’ everything changed. It’s not about the pill. It’s about the person holding it.
On January 10, 2026 AT 14:43
Molly McLane
Just had a 78-year-old woman ask me why her new generic lisinopril was blue instead of white. She’d been on the white one for 12 years. I showed her the FDA page, printed out the bioequivalence chart, and told her, ‘This pill is your old pill’s twin. Same DNA. Just different clothes.’ She hugged me. Then asked if I could write a note so her granddaughter could understand too. That’s the real work.
On January 11, 2026 AT 05:26
Stuart Shield
It’s like buying a BMW engine and getting a Honda that runs just as well - but the hood doesn’t have the logo. People don’t hate the engine. They hate not knowing it’s the same. We’ve turned medicine into a status symbol. And now we’re surprised when folks cling to the badge instead of the function. We need to stop selling pills and start selling trust.
On January 11, 2026 AT 12:58
Amy Le
Generics are a socialist plot to make Americans take cheap medicine while the elites keep their brand-name vitamins. The FDA? Controlled by Big Pharma. My cousin’s aunt’s neighbor’s dog got sick after a generic. Coincidence? I think not. Pay more. Stay safe. America First.
On January 13, 2026 AT 04:58