Every year, thousands of people end up in the emergency room because of something they didn’t tell their doctor: the vitamins, herbs, or painkillers they’re taking on their own. You might think, It’s just a multivitamin or I’m only taking fish oil for my joints. But what you don’t know is that your fish oil could be making your blood thinner than your doctor thinks - and that could be dangerous if you’re on warfarin. Or that the St. John’s Wort you take for mood could knock out the effectiveness of your birth control or antidepressant. The problem isn’t the supplement. It’s the silence.
Why Your Provider Needs to Know What You’re Taking
The U.S. dietary supplement market hit $57.8 billion in 2022. Nearly 8 out of 10 Americans take at least one supplement. But only 36% of them tell their doctor. That’s not a small oversight. That’s a safety gap wide enough to drive a truck through. The FDA doesn’t approve supplements before they hit the shelf like it does with prescription drugs. That means there’s no guarantee what’s in the bottle matches what’s on the label. A 2022 Government Accountability Office report found that 23% of supplement labels had wrong ingredient amounts or even included unlisted substances. One person might take a turmeric capsule labeled "500mg," but it could actually contain 700mg - or worse, a hidden stimulant. And here’s the real risk: supplement-drug interactions. A 2021 study in JAMA Internal Medicine found that 23% of hospital patients had potential interactions between their prescriptions and supplements. Nearly 8% of those were classified as severe - meaning they could lead to liver failure, dangerous bleeding, or heart rhythm problems. The FDA recorded 1,034 adverse events linked to supplements in 2022, including 52 deaths. Many of those could have been avoided if someone had simply said, "I take kava every night."What Counts as a Supplement - And What Doesn’t
Not everything you take is obvious. You might think of supplements as pills you buy at the health food store. But here’s the truth: if it’s not a prescription drug and it’s not food, and it’s meant to affect your body’s function - it’s a supplement. That includes:- Vitamins (like vitamin D, B12)
- Minerals (magnesium, zinc, calcium)
- Herbs (echinacea, ginkgo, ashwagandha)
- Probiotics and prebiotics
- Omega-3s and fish oil
- Protein powders and meal replacements
- Energy boosters, sleep aids, or weight loss formulas
How to Keep an Accurate Record
You can’t remember everything. And your provider won’t ask unless you bring it up. So you need a system. The National Institutes of Health Office of Dietary Supplements (NIH ODS) created a simple form called My Dietary Supplement and Medicine Record. Use it. Print it. Fill it out. For every product, write down:- Name: Exact brand and product name. Not "vitamin C." Write "Nature Made Vitamin C 500mg Tablets."
- Dose: How much? 500mg? 1,000mg? 1 capsule? 2 teaspoons?
- Frequency: Once a day? Twice a day? After meals? Before bed?
- Purpose: Why are you taking it? "For joint pain," "for sleep," "for immune support" - be specific.

When and How to Bring It Up
Most providers don’t ask. That’s the sad truth. A 2022 study found that over half of patients who didn’t disclose supplements said their provider never asked. So don’t wait. Bring it up yourself. Start with your next appointment. Say this: "I want to make sure you know everything I’m taking. I’ve been using [list products] for [reason]. I’m not sure if they interfere with my other meds. Can we check?" You don’t need to be embarrassed. You’re not being difficult. You’re being smart. Providers who ask about supplements get 4.7 out of 5 patient satisfaction ratings. Those who don’t? 3.2. Patients notice. And they reward the ones who care. If you’re seeing a new doctor, bring your list with you. If you’re getting a lab test or surgery, mention it again. Even if you’ve told them before - things change. You might have started a new supplement last week. That matters.What Your Provider Should Do
It’s not just your job. Providers need to be better too. The American Medical Association says clinicians should ask about supplements at every visit - not just when they think it’s relevant. Pharmacists are especially good at catching interactions. One study found they identify 3.2 times more potential problems than physicians during medication reviews. But here’s the catch: most electronic health records (EHRs) still don’t have a dedicated field for supplements. A 2021 study found only 31% of primary care EHRs let providers log supplements separately. That means your fish oil might get lumped in with "other meds" - and overlooked. That’s changing. Epic Systems, the biggest EHR company in the U.S., added specific supplement fields in 2020. Their 2024 update will include AI that scans for interactions between 14,700 supplements and prescriptions. But until every clinic uses this, you still need to speak up.Common Mistakes People Make
You’re not alone if you’ve made one of these:- "It’s natural, so it’s safe." Kava and comfrey are natural. They’ve caused liver failure. "Natural" doesn’t mean harmless.
- "I only take it once in a while." Even occasional use can interact. A single dose of St. John’s Wort can reduce the effectiveness of birth control for up to two weeks.
- "I didn’t think it was important." That’s the #1 reason people don’t disclose - 63% of users in a Consumer Reports survey said this. But if it’s affecting your body, it’s important.
- "My doctor never asked." That’s not your fault. But it’s still your responsibility to speak up.
- "I just take what’s on the label." Labels aren’t always accurate. A 2022 GAO report found nearly a quarter of supplement labels were wrong.
Real Stories - What Happens When People Don’t Talk
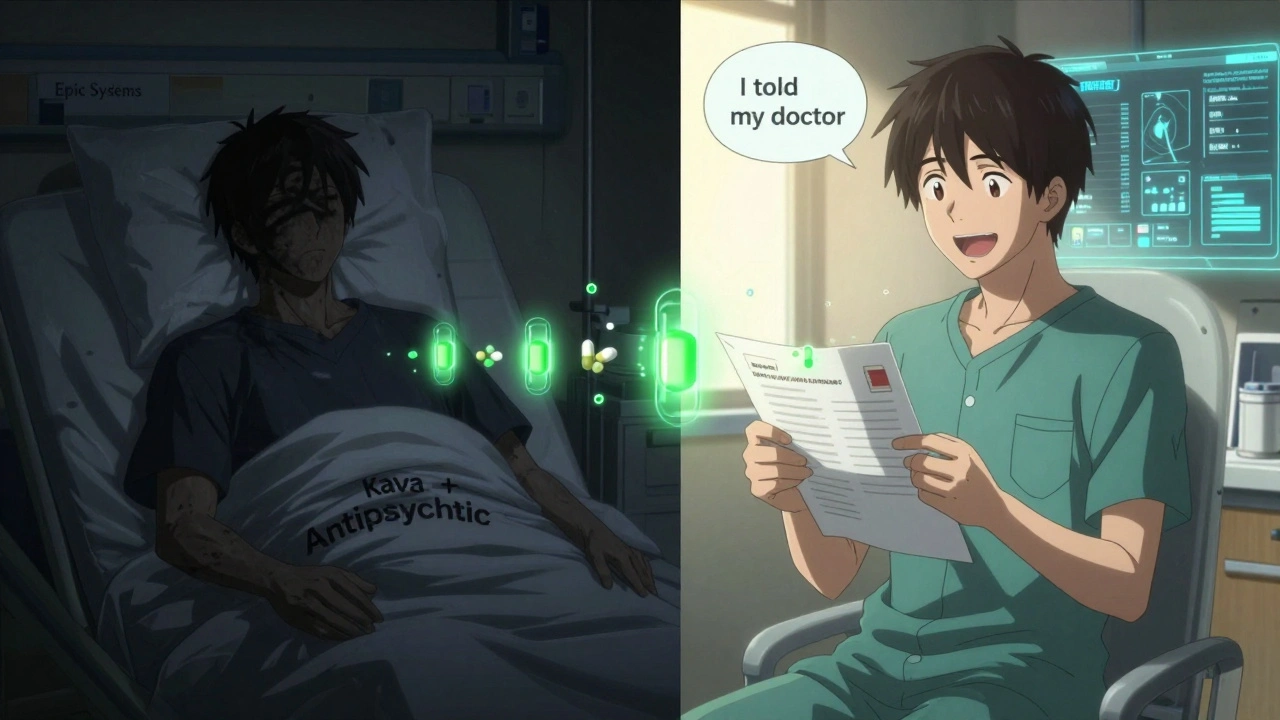
In 2019, a 45-year-old woman died from acute liver failure. She was taking kava for anxiety and an antipsychotic medication. Her doctors never knew about the kava. The autopsy revealed it. On the other side, a 68-year-old woman avoided a dangerous bleed because she mentioned her 1,000mg daily fish oil dose during a routine check-up. Her warfarin dose was lowered before it became a crisis. These aren’t rare. They’re preventable.What You Can Do Today
You don’t need to wait for your next appointment. Here’s your action plan:- Go through your medicine cabinet. Pull out every bottle - vitamins, herbs, OTC painkillers, sleep aids, protein powders.
- Write down the exact name, dose, frequency, and reason for each.
- Take a photo of each Supplement Facts or Drug Facts label.
- Bring this list to your next visit - even if it’s just for a flu shot.
- Ask: "Could any of these interact with my other medications?"
Bottom Line
Your health isn’t just about your prescription. It’s about everything you put into your body. Supplements aren’t harmless. OTC drugs aren’t trivial. The gap between what you take and what your provider knows is where mistakes happen. You don’t need to be an expert. You just need to be honest. And you need to be proactive. The system isn’t perfect. But you can be.Do I need to tell my doctor about vitamins and minerals?
Yes. Vitamins and minerals are dietary supplements, and they can interact with prescription drugs. For example, vitamin K can reduce the effect of blood thinners like warfarin. Calcium can interfere with thyroid medication. Even a daily multivitamin can affect lab results or drug absorption. Always list them.
What if my provider says supplements aren’t important?
Some providers still don’t prioritize supplement use - but that doesn’t mean it’s safe to skip telling them. If your provider dismisses your concerns, say: "I’ve read that interactions can be serious, and I want to make sure I’m not at risk." If they still don’t listen, consider finding a provider who takes a more comprehensive approach. Your safety matters more than their opinion.
Can I just tell my pharmacist instead?
Yes - and you should. Pharmacists are trained to catch drug-supplement interactions. Many offer free medication reviews. Bring your list to your pharmacy every time you fill a new prescription. They can flag risks your doctor might miss, especially if your EHR doesn’t track supplements well.
Are herbal supplements riskier than vitamins?
Herbal supplements carry higher risks because they contain complex plant chemicals that can act like drugs. St. John’s Wort, for example, affects liver enzymes that break down over 30 medications, including antidepressants, birth control, and chemotherapy drugs. Vitamins are generally safer in standard doses, but high doses (like 1,000mg+ of vitamin C or E) can still interfere with treatments or cause toxicity.
What if I’m taking a supplement for a medical condition?
That’s even more reason to tell your provider. If you’re using turmeric instead of anti-inflammatory meds, or melatonin instead of a sleep prescription, your provider needs to know. They can’t manage your condition safely if they don’t know what you’re doing. Some supplements can help - but only when used correctly and monitored.

Comments
Gillian Watson
I just started listing everything I take in my phone notes after reading this. Turns out I was taking three things that could mess with my blood pressure med and never knew. Scary stuff.
Now I show my pharmacist every time I pick up a script.
On December 4, 2025 AT 21:20
Martyn Stuart
Let me be very clear: if you're taking anything that isn't a prescription drug, and it's meant to alter your physiology-whether it's a capsule, a powder, or a tea-you're taking a supplement. And yes, that includes your 'natural' green tea extract, your 'harmless' magnesium, and your 'just for sleep' melatonin. These are pharmacologically active substances, and they interact with your medications in ways that are not always predictable, not always documented, and not always visible until it's too late. The FDA doesn't regulate them like drugs, so the burden of safety falls entirely on you. Keep a written log. Bring it to every appointment. Don't assume your doctor knows. They don't. And if they don't ask, they're not doing their job properly. Your life isn't a gamble.
On December 5, 2025 AT 15:14
Shofner Lehto
I work in a clinic and we’ve started using the NIH form for every new patient. It’s changed everything. Before, we’d miss half the supplements. Now, we caught a patient on St. John’s Wort who was about to have a serotonin crisis with his SSRI. He didn’t think it was a big deal because it was ‘herbal.’ We saved him. Just ask. Just list it. It’s not awkward-it’s smart.
On December 6, 2025 AT 02:27
Chase Brittingham
This post hit me hard. I’ve been taking ashwagandha for stress for two years. Never told my cardiologist. I just figured, it’s natural, right? Turns out it can raise blood pressure in some people-and I’ve got hypertension. I just printed out the NIH form and I’m bringing it to my next appointment. No more guessing. No more silence. Thanks for this.
On December 7, 2025 AT 02:59
Bill Wolfe
It's frankly embarrassing that people still think 'natural' means 'safe.' You're not a caveman with a handful of leaves. You're a modern human with access to science, data, and evidence-based medicine-and yet you're still swallowing mystery powders labeled 'Turmeric Supreme' because some influencer on Instagram said it 'cleanses your chakras.' If you're going to ingest something that affects your biochemistry, you owe it to yourself and your provider to know exactly what it is, what it does, and what it might kill. And if your doctor doesn't care? Find a new one. This isn't about being paranoid-it's about not being a statistic.
On December 7, 2025 AT 08:43
michael booth
I appreciate this post. It’s clear, practical, and urgently needed. I’ve been encouraging my patients to maintain a supplement log for years. The NIH form is excellent. I also recommend taking a photo of each label. It eliminates guesswork. And yes, even your multivitamin matters. A daily 1,000 IU of vitamin D can interfere with certain heart medications. A single gram of calcium can affect thyroid absorption. These are not trivial details. They are clinical facts. Please, take five minutes and document everything. Your life depends on it.
On December 7, 2025 AT 22:21
Rudy Van den Boogaert
My mom died from liver failure after taking kava. She never told her doctor because she thought it was just a herbal relaxant. I didn’t even know she was taking it until the autopsy. I wish I’d known. I wish she’d known. Please don’t make the same mistake. Write it down. Tell someone. It’s not about being dramatic. It’s about being alive.
On December 8, 2025 AT 13:11
Yasmine Hajar
My doctor told me supplements were a waste of money. So I stopped telling him. Then I started taking melatonin for sleep and got a weird heart flutter. My pharmacist noticed it when I filled my beta-blocker. He asked about supplements. I said yes. He checked the interaction. Turns out melatonin can increase heart rhythm risk with beta-blockers. I almost didn’t say anything because I thought my doctor already knew. He didn’t. I’m not ashamed to say I was dumb. Now I bring my list every visit. Even for a cold. Even for a flu shot. I’m done being quiet about what’s in my body.
On December 10, 2025 AT 04:25