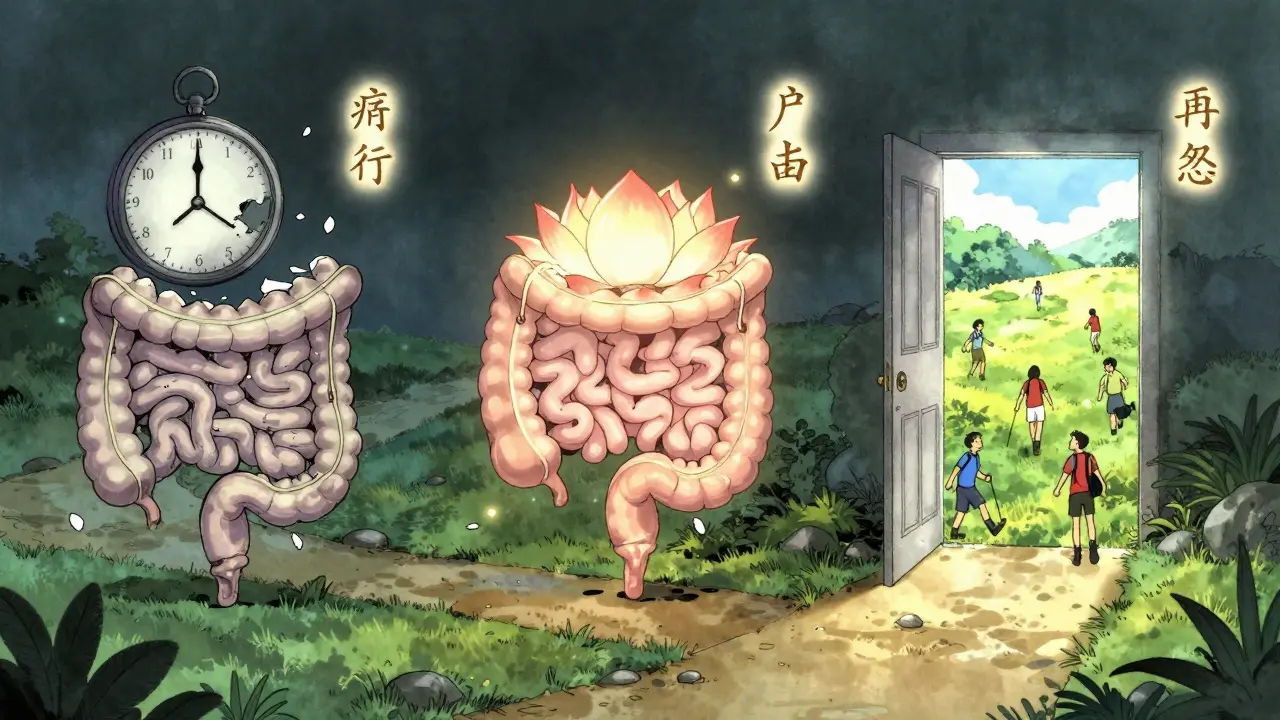
When IBD Medications Don’t Work, Surgery Becomes the Next Step
For people with Crohn’s disease or ulcerative colitis, medication can help control inflammation, reduce symptoms, and keep flare-ups at bay. But what happens when drugs stop working? When you’re having constant diarrhea, severe abdominal pain, rectal bleeding, or dangerous complications like bowel blockages or toxic megacolon, surgery isn’t a last resort-it’s often the only way to regain control of your life. About 75% of people with Crohn’s and up to 30% of those with ulcerative colitis will eventually need surgery. It’s not about failure; it’s about finding a better path forward.
What Does IBD Surgery Actually Involve?
IBD surgery isn’t one single procedure. It’s a set of options chosen based on your disease type, location, and overall health. The two main goals are to remove damaged tissue and restore or redirect bowel function.
Bowel resection is common in Crohn’s disease. If a section of your small intestine or colon is severely inflamed or scarred, surgeons cut it out and reconnect the healthy ends. This is called anastomosis. It’s usually done laparoscopically-through small keyhole incisions-so recovery is faster. Hospital stays average 3 to 5 days. But here’s the catch: Crohn’s doesn’t cure itself. Even after removing the bad part, the disease can come back nearby. Studies show 80% of patients see it return within 10 years without ongoing medication.
Colectomy removes part or all of the colon. For ulcerative colitis, this is often the goal because the disease only affects the colon and rectum. Once those are gone, the disease is gone too. No more bloody stools. No more urgent bathroom trips. That’s why many people with ulcerative colitis feel like they’ve been given a second chance after surgery.
The J-Pouch: A Natural Alternative to an Ostomy
One of the biggest advances in IBD surgery is the ileal pouch-anal anastomosis, or IPAA-commonly called the J-pouch. Instead of creating a permanent opening in the abdomen (an ostomy), surgeons use the last 8 to 10 centimeters of your small intestine to build a small internal pouch shaped like a J. This pouch is connected directly to your anus. You still go to the bathroom normally, just more often.
Most people with a J-pouch have 4 to 8 bowel movements a day after recovery. That’s more than before surgery, but far fewer than during a flare. Around 80 to 90% of patients report high satisfaction with this option. The pouch acts like a reservoir, storing stool so you don’t have to rush to the toilet constantly.
But it’s not simple. J-pouch surgery usually happens in three stages:
- First, the colon and rectum are removed, and a temporary ileostomy is created.
- After 8 to 12 weeks, the pouch is built and connected to the anus. The stoma stays in place to let the new connection heal.
- Finally, the temporary stoma is closed. You’re back to using your anus.
Each stage means another hospital stay and recovery period. About 60% of people get a temporary stoma. Complications like leaks at the connection site happen in 5 to 15% of cases and can be serious. That’s why surgeons often choose to go slow-protecting the new pouch is more important than rushing to close the stoma.

When an Ostomy Is Necessary
Not everyone is a candidate for a J-pouch. If your anal sphincter is damaged, if you’re over 70, or if you’re a woman planning to get pregnant, your doctor might recommend a permanent ileostomy instead. In this procedure, the end of your small intestine is brought out through your abdomen. Waste collects in a bag you wear outside your body.
The stoma is about the size of a quarter, sticking out 1 to 2 centimeters from your skin. You’ll need to empty the bag 4 to 6 times a day. It sounds daunting, but many people say it’s life-changing. One Reddit user wrote: “I went from 15 bathroom trips a day to zero anxiety. I can travel, sleep through the night, and hug my kids without fear.”
Permanent ostomies are also common after Crohn’s surgery if the rectum is involved, or if the J-pouch fails. About 10% of people who get a J-pouch end up needing a permanent stoma later due to complications like chronic pouchitis or fistulas.
There are no “good” or “bad” options here-just different trade-offs. A J-pouch means no external bag but more internal complications. An ostomy means no internal risks but a visible appliance. Both eliminate colorectal cancer risk completely.
What Happens After Surgery? The Real Recovery
Surgery isn’t the end-it’s the start of a new routine. Recovery takes months, not weeks. The first 6 to 12 months are the hardest. Your body is learning how to handle the new setup.
If you have a J-pouch, you’ll likely have 6 to 10 bowel movements a day at first. That drops to 4 to 8 as your pouch stretches and adapts. You’ll need to drink 8 to 10 cups of fluid daily to avoid dehydration. High-fiber foods like nuts, seeds, and raw vegetables can block your pouch early on. Stick to soft, low-residue meals until your surgeon says otherwise.
If you have an ostomy, you’ll need to learn how to change your bag, care for the skin around your stoma, and prevent leaks. Skin irritation is the most common complaint. A good ostomy nurse can teach you how to use barrier creams, proper adhesive techniques, and belt supports to keep things secure. Products like the Convatec Adapt Mini Belt cost around $46 and help prevent bag droop during movement.
One of the biggest surprises for many patients is pouchitis-inflammation of the J-pouch. It affects up to 40% of people within a few years. Symptoms include increased bowel movements, cramping, and sometimes fever. It’s usually treated with antibiotics like ciprofloxacin. Some people need long-term low-dose antibiotics to keep it under control.
Who Shouldn’t Get a J-Pouch?
Not everyone is a candidate. Your surgeon will screen you carefully. You might not be eligible if:
- You have severe damage to your anal sphincter (can’t control bowel movements)
- You’re a woman planning pregnancy-J-pouch surgery increases infertility risk from 15% to 50-70%
- You’re a man concerned about sexual function-up to 20% develop new erectile dysfunction after surgery
- You’re over 70 and have other health issues-complication risks rise with age
- You have Crohn’s disease affecting the pouch area-recurrence rates are too high
For these people, a permanent ileostomy is often the safer, more reliable choice. There’s no shame in it. Many people with permanent stomas live full, active lives-hiking, swimming, working, raising families.
What’s New in IBD Surgery?
Technology is making surgery safer and recovery faster. Laparoscopic (keyhole) surgery is now the standard-used in 65% of cases. Robotic-assisted surgery is growing fast. At Mayo Clinic, robotic IPAA procedures have 15% fewer complications and 20% shorter operating times than traditional laparoscopic ones.
Smart ostomy bags are now available. The OstoLert by ConvaTec, approved by the FDA in mid-2023, has sensors that alert your phone if the bag is about to leak. It costs around $80, but for many, it’s worth it for peace of mind.
Researchers are also testing ways to prevent pouchitis. A major NIH-funded trial is looking at fecal microbiota transplants-giving patients healthy gut bacteria from donors. Early results show a 40% drop in pouchitis after one year. That could change how we manage long-term care.
Support Is Key-You’re Not Alone
Recovery isn’t just physical. It’s emotional. Many people feel self-conscious about their stoma or worry about how others will react. That’s why support groups matter. Online communities like r/IBD on Reddit have over 28,000 members. The United Ostomy Associations of America connects thousands with peer mentors.
Before surgery, ask for a certified wound, ostomy, and continence nurse (WOCN). They’ll teach you everything-from how to change a bag to what foods to avoid. Most hospitals offer 3 to 5 training sessions. Don’t skip them. This is the difference between struggling and thriving.
And remember: 68% of J-pouch patients are readmitted within 90 days, mostly for dehydration or pouchitis. That doesn’t mean you failed. It means you need to be prepared. Keep a symptom journal. Know your warning signs: fever over 101°F, output over 1,500 mL a day, or sudden worsening pain.
Surgery Doesn’t Mean the End-It Means a New Beginning
IBD surgery isn’t about giving up on medicine. It’s about switching strategies. For many, it’s the moment they finally breathe easy. No more hiding. No more panic. No more endless cycles of flare-ups and hospital visits.
Success rates are high. Eighty-five percent of people with permanent ostomies are satisfied five years later. For J-pouch patients, it’s 78%. Both options give you back your life. The choice isn’t about which is better-it’s about which fits you.
If you’re considering surgery, talk to an IBD specialist. Ask about your options. Ask about risks. Ask about life after. You’re not just choosing a procedure-you’re choosing a future where your body works for you, not against you.
Is IBD surgery a cure for ulcerative colitis?
Yes, for ulcerative colitis, removing the entire colon and rectum (proctocolectomy) is the only known cure. Since the disease only affects the colon and rectum, removing those organs eliminates the source of inflammation. You’ll no longer have bloody stools, urgent diarrhea, or cancer risk from long-standing colitis. However, if you have a J-pouch, you can still develop pouchitis, which is inflammation of the new internal pouch-not the original disease.
Can I still have children after J-pouch surgery?
Women who have J-pouch surgery face a higher risk of infertility. Studies show infertility rates jump from about 15% before surgery to 50-70% afterward. This is due to scar tissue formation in the pelvis and changes to reproductive anatomy. If you plan to have children, talk to your surgeon before surgery. Some women opt for egg freezing before the procedure. Men may experience erectile dysfunction in up to 20% of cases, often due to nerve damage during surgery.
How often do I need to empty an ileostomy bag?
Most people empty their ileostomy bag 4 to 6 times a day. Output is typically liquid or semi-liquid because the colon, which absorbs water, has been removed. You’ll need to carry supplies with you when you’re out. The bag should be emptied when it’s about one-third full to prevent leaks and reduce weight pulling on the skin. Modern bags are discreet and odor-free, and many people forget they’re wearing one after a few weeks.
What are the biggest risks after IBD surgery?
The most serious risks include anastomotic leak (where the reconnected bowel sections don’t heal properly), infection, and blood clots. For J-pouch patients, pouchitis affects up to 40% and can require long-term antibiotics. Strictures (narrowing) and fistulas (abnormal connections) can also develop. About 25% of people who undergo three-stage J-pouch surgery face complications. Temporary ostomies help reduce leak risks, which is why surgeons often recommend them even if a permanent stoma isn’t planned.
Will I need to take medication after surgery?
Yes, especially if you have Crohn’s disease. Even after removing diseased bowel, Crohn’s can return in other areas. Most patients continue taking maintenance medications like biologics or immunomodulators to prevent recurrence. For ulcerative colitis patients with a J-pouch, some doctors recommend low-dose mesalamine to reduce pouchitis risk. For those with a permanent stoma, medication is usually stopped unless there are other conditions like small bowel Crohn’s.


Comments
Chloe Hadland
I had my J-pouch done 3 years ago. The first 6 months were hell, but now I can run 5Ks and eat tacos without panic. This post nailed it. You're not broken-you're rebuilt.
On January 24, 2026 AT 21:54
Amelia Williams
I’m pre-op next month and I’ve been reading every thread I can find. The part about hydration being non-negotiable? Game changer. I’ve already started chugging water like it’s my job.
On January 26, 2026 AT 07:18
Alexandra Enns
This is why Canada’s healthcare is superior. You people in the US are still debating if a smart ostomy bag is worth $80? We get it covered. Also, why is everyone acting like pouchitis is some new horror story? It’s 2024, we have antibiotics. Stop dramatizing.
On January 27, 2026 AT 13:14
Heather McCubbin
I read this whole thing and still think people are too quick to cut things out. Your body is not a machine you can upgrade. You’re just trading one set of problems for another. Why not try fasting? Or turmeric? Or just... believing harder?
On January 28, 2026 AT 11:34
Tiffany Wagner
I had a permanent stoma after 12 years of UC. No one tells you how much you miss feeling like a person instead of a symptom. The bag? It’s just a tool. I wear shorts now. I swim. I hug my niece. It’s not perfect but it’s mine.
On January 29, 2026 AT 02:23
Viola Li
If you're getting surgery because you 'can't handle your life' maybe you need therapy not a colectomy. I mean really. 75% of Crohn's patients? That's just giving up. You're not sick you're weak.
On January 30, 2026 AT 07:31
Himanshu Singh
Bro. I had my J-pouch at 29. Now I'm 37. I’ve had 3 pouchitis flares. Took cipro each time. Still go 5x a day. Still travel solo. Still date. Still laugh. This isn’t the end. It’s the start of your real life. You got this.
On January 31, 2026 AT 17:39
lorraine england
Just want to say the part about the Convatec belt? Lifesaver. I bought one after my second leak disaster. Worth every penny. Also, if you’re scared of changing your bag, just do it in the shower. No shame. We’ve all been there.
On February 2, 2026 AT 11:09
Jamie Hooper
I had the surgery in 2021 and now I'm basically a human WiFi router with a bag attached. The OstoLert thing? Sounds like a scam. But I'm still here. Still alive. Still kinda weirded out by how normal I feel now.
On February 3, 2026 AT 18:17