Local Anesthesia Dosage Calculator
Maximum Safe Dose
mg
Estimated Duration
minutes
How It Works
Local anesthesia dosing is calculated based on patient weight and the specific agent used. The maximum dose is typically calculated in mg/kg of body weight.
Lidocaine: Maximum dose is 4.5 mg/kg (max 300 mg)
Articaine: Maximum dose is 7 mg/kg (max 500 mg)
Epinephrine (1:100,000) extends duration but doesn't affect the maximum dose calculation.
Ever wondered why you feel nothing when a dentist pulls a tooth or stitches a gum? The secret is local anesthesia, a technique that numbs a tiny area while you stay fully awake. In oral surgery, that numbness can make the difference between a smooth, painless experience and a stressful one. Below you’ll learn exactly how it works, which drugs are best, and what you should watch out for before and after the procedure.
Key Takeaways
- Local anesthesia blocks nerve signals in the mouth, letting surgeons work without causing pain.
- Lidocaine and articaine are the two most common agents; articaine often has a faster onset.
- Choosing between infiltration and nerve block depends on the surgical site and patient anatomy.
- Dosage, epinephrine add‑on, and patient health conditions determine safety and effectiveness.
- Knowing the signs of complications helps you act quickly if something goes wrong.
What Is Local Anesthesia?
Local anesthesia is a medical technique that temporarily blocks nerve transmission in a specific area of the body, allowing procedures to be performed without pain while the patient stays conscious. In dentistry it’s delivered by injection into the tissues surrounding teeth, gums, or the jawbone. Unlike general anesthesia, it doesn’t affect breathing or heart rate, which makes it safer for most outpatient surgeries.
Why It Matters in Oral Surgery
Oral surgery is any surgical procedure that involves the mouth, jaws, teeth, or related facial structures, ranging from simple tooth extractions to complex implant placements. Because the mouth is densely innervated-meaning lots of nerves run close together-precise numbness is essential. Without it, patients would feel every incision, bone cutting, or suture placement, turning a routine extraction into a traumatic event.
How Local Anesthesia Works in the Mouth
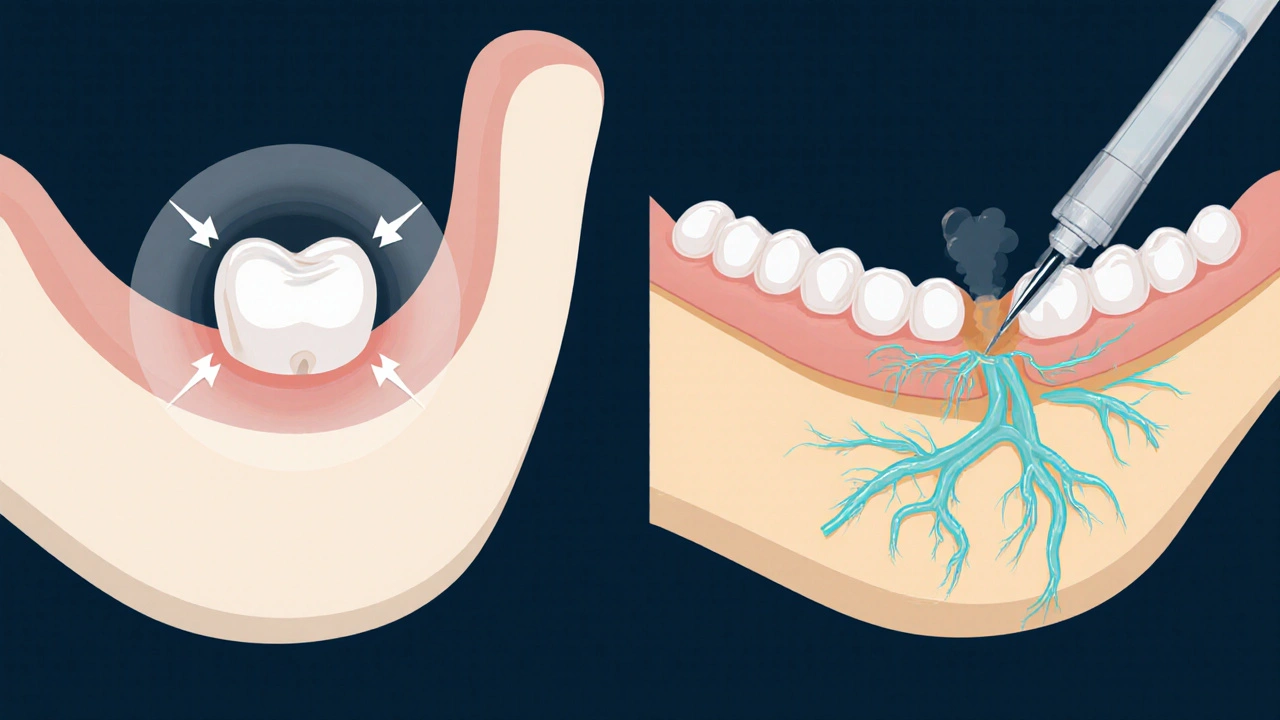
The drug targets sodium channels on nerve fibers, stopping the electrical impulses that signal pain to the brain. In dental practice, the most reliable way to reach those nerves is through a nerve block an injection that surrounds a major nerve trunk, typically the inferior alveolar, mental, or lingual nerve, to numb an entire quadrant of the mouth. For smaller areas, an infiltration a technique that injects anesthetic directly into the tissue surrounding a single tooth or small region, providing focused numbness. Both methods rely on the same chemistry but differ in depth and spread.
Choosing the Right Anesthetic Agent
The two workhorses in dental clinics are lidocaine and articaine. Below is a side‑by‑side look at their key attributes.
| Attribute | Lidocaine | Articaine |
|---|---|---|
| Typical concentration | 2% (often with 1:100,000 epinephrine) | 4% (often with 1:100,000 epinephrine) |
| Onset time | 2-3 minutes | 1-2 minutes |
| Duration (without epinephrine) | 60-90 minutes | 75-120 minutes |
| Maximum adult dose | 4.5mg/kg (max 300mg) | 7mg/kg (max 500mg) |
| Special notes | Very well‑studied, reliable for all ages | Higher lipid solubility; penetrates bone better, but avoid in patients with severe allergy to amide anesthetics |
Both drugs are classified as amide‑type local anesthetics a class of anesthetic agents characterized by a chemical structure that includes an amide bond, providing longer duration and lower toxicity compared to ester‑type agents. The choice often comes down to the surgeon’s preference, the specific procedure, and patient factors.
When to Use Infiltration vs. Nerve Block
For a single‑tooth extraction in the upper jaw, a simple infiltration is usually enough. The maxillary bone is porous, allowing the anesthetic to diffuse quickly. In contrast, lower‑jaw work-especially on molars-benefits from an inferior alveolar nerve block because the dense mandibular bone prevents effective infiltration.
- Infiltration: Ideal for front teeth, shallow procedures, patients with anxiety about deep injections.
- Nerve block: Best for multi‑tooth extractions, implant placement, or any surgery that involves the posterior mandible.
Dosage, Onset, and Duration - Practical Guidelines
Understanding the numbers helps you avoid under‑ or over‑dosing. Here’s a quick cheat sheet:
- Calculate the maximum safe dose based on the patient’s weight (e.g., 4.5mg/kg for lidocaine).
- Add epinephrine (1:100,000) unless the patient has a contraindication; it slows absorption, extending the block up to three‑fold.
- Inject slowly-about 1mL per 30 seconds-to reduce the risk of vascular uptake and bruising.
- Test the numbness after 2-3 minutes (lidocaine) or 1-2 minutes (articaine) before starting the surgery.
- Document the exact amount used; if the procedure drags on, you can safely supplement with a second cartridge within the adult maximum.

Safety, Contraindications, and Side Effects
Local anesthesia is safe, but certain conditions require caution:
- Allergy to amide anesthetics: Rare, but presents as rash, itching, or anaphylaxis. If suspected, avoid lidocaine and articaine and opt for an ester‑type like procaine.
- Cardiovascular disease: Epinephrine can raise heart rate and blood pressure. Use a lower concentration (1:200,000) or plain anesthetic.
- Pregnancy: Lidocaine is Category B (generally safe); articaine is also considered low risk, but dose should be minimized.
- Pregnancy: Use minimal effective volume and avoid high‑dose epinephrine.
Common, transient side effects include lip or cheek numbness longer than the procedure, mild swelling at the injection site, and a metallic taste. More serious but rare complications are:
- Intravenous injection leading to tachycardia (usually from accidental intravascular placement).
- Hematoma formation if a blood vessel is punctured.
- Persistent paresthesia-numbness that lasts weeks-most often after a nerve block.
Regulatory bodies such as the FDA the U.S. Food and Drug Administration, responsible for ensuring the safety and efficacy of drugs and medical devices require manufacturers to list maximum dosages and contraindications on the label, and the AAOMS the American Association of Oral and Maxillofacial Surgeons, a professional organization that publishes clinical guidelines for oral surgery practices recommends adhering strictly to those limits.
Patient Experience: What to Expect Before, During, and After
Before: Your surgeon will review your medical history, ask about any allergies, and possibly request a blood pressure check if epinephrine is planned. You’ll be seated upright, and a topical anesthetic gel may be applied to the gum to ease the initial needle poke.
During: You’ll feel a brief pressure as the syringe penetrates tissue, followed by a cooling sensation. Within minutes, the area becomes numb-often described as “pins and needles” that fade away.
After: Numbness can linger for 2-4 hours, depending on the drug and whether epinephrine was used. During this window, avoid chewing hot foods or speaking loudly to prevent accidental bites. Ice packs can reduce swelling; over‑the‑counter ibuprofen manages mild pain that emerges once the block wears off.
Tips for a Smooth Recovery
- Keep your head elevated for the first 24hours to limit swelling.
- Soft foods (yogurt, mashed potatoes) are best until full sensation returns.
- Gentle rinses with warm salt water after the first 24hours help keep the site clean.
- Contact your surgeon if numbness lasts more than 8hours or if you notice persistent tingling, sharp pain, or swelling.
Frequently Asked Questions
How long does a local anesthetic actually numb the area?
With 1:100,000 epinephrine, lidocaine typically lasts 2-3hours, while articaine can extend up to 4hours. Duration shortens if the patient is very active or if the injection is placed near a large blood vessel.
Can I be allergic to lidocaine?
True allergy to amide anesthetics like lidocaine is rare (<0.1% of patients). Most reactions are due to preservatives or epinephrine. A skin prick test can confirm the cause.
Is it safe to have a nerve block if I have high blood pressure?
Yes, but the dentist should use a lower epinephrine concentration (1:200,000) or a plain anesthetic. Monitoring during the procedure is recommended.
Why does my cheek feel numb for longer than my tooth?
In a mandibular nerve block, the anesthetic spreads to the surrounding soft tissue, which often retains the drug longer than the dense bone around the tooth.
Can I take painkillers while the anesthesia is still active?
Over‑the‑counter NSAIDs (ibuprofen or naproxen) are safe and can actually improve comfort once the numbing wears off. Avoid aspirin if you’re on blood thinners.
Local anesthesia may sound technical, but it’s essentially a carefully measured numbing “switch” that lets oral surgeons work efficiently while you stay fully aware. Knowing the drugs, techniques, and safety steps empowers you to ask the right questions and recover confidently.


Comments
Kim and Lin
Just had a molar pulled last week and the numbing felt like magic – no pain, just that weird tingly vibe, and it totally reminded me why this guide is gold. 😊
Never realized how much the epinephrine dosage matters until I felt the difference in the recovery.
On October 12, 2025 AT 21:08
Kemari Nielson
The dosage tables are accurate; always calculate mg/kg and stay below the listed maximum.
On October 17, 2025 AT 12:15
Terry Washington
One must appreciate that the very foundation of contemporary oral surgery rests upon a nuanced understanding of pharmacokinetics, a fact that this guide so eloquently elucidates. The distinction between lidocaine and articaine is not merely academic; it reflects a divergence in lipid solubility that directly influences bone penetration efficacy. When one considers the electrophysiological blockade of sodium channels, the narrative transcends simple numbing to embrace the art of selective neuronal inhibition. Moreover, the inclusion of epinephrine as an adjuvant is a masterstroke, extending duration while modulating systemic absorption-a principle that echoes the broader tenets of anesthetic stewardship. The guide’s insistence on weight‑based dosing safeguards against iatrogenic toxicity, a paramount concern in patients with comorbidities. It is commendable that the authors reference FDA and AAOMS guidelines, anchoring practice in regulatory rigor. Additionally, the discussion of contraindications, especially in cardiovascular disease, demonstrates a holistic patient‑centric approach. The tabular comparison, though succinct, conveys critical variables such as onset time, peak effect, and maximum safe thresholds, enabling clinicians to make informed decisions swiftly. By demystifying the decision matrix between infiltration and nerve block, the article empowers practitioners to tailor techniques to anatomical nuances-an essential skill in the management of posterior mandibular extractions. The emphasis on slow injection speed to mitigate vascular uptake underscores a refined awareness of iatrogenic complications like hematoma formation. Furthermore, the post‑operative care recommendations, such as head elevation and soft‑diet protocols, reflect an evidence‑based continuum of care. In an era where patient satisfaction metrics dominate practice viability, such comprehensive guidance is indispensable. Finally, the inclusion of a JavaScript calculator, while perhaps superfluous to some purists, showcases an innovative attempt to integrate digital tools into clinical decision‑making, a forward‑looking gesture that cannot be dismissed. In summation, this guide epitomizes the synthesis of scientific precision and practical applicability, setting a benchmark for future educational endeavors in dental anesthesia.
On October 21, 2025 AT 21:48
Claire Smith
The article is thorough, though the use of dense technical jargon may alienate lay readers seeking simple explanations.
On October 26, 2025 AT 01:48
fred warner
Great read!
On October 29, 2025 AT 23:15
Veronica Mayfair
Yo! This guide is lit 🔥. Love the vibes and the emojis, even if I wiked a few spellings. Keep it up! 😁
On November 2, 2025 AT 16:08
Rahul Kr
Cool stuff. I mostly just skimmed the dosage part, but the tips on post‑op care are handy.
On November 6, 2025 AT 03:28
Anthony Coppedge
Excellent breakdown; the step‑by‑step dosage calculation is clear, and the recommendation to inject 1 mL per 30 seconds minimizes intravascular risk. Also, the reminder to test sensation after 1–2 minutes is spot‑on. One tiny suggestion: a quick note on the maximum cumulative dose when using multiple cartridges could further prevent accidental overdosing.
On November 9, 2025 AT 09:15
Nicholas Blackburn
Honestly, if you’re still reading this you’re probably scared of a needle. Get over it, the numbness is nothing but a mild tingle.
On November 12, 2025 AT 09:28
Dave Barnes
One could argue that the philosophical underpinnings of anesthesia are akin to the ancient quest for balance-silencing pain while preserving consciousness. Yet the practical aspects dominate, and this guide nails that balance.
On November 15, 2025 AT 04:08
Kai Röder
Thanks for the comprehensive guide. The clear headings make it easy to find the info you need, and the safety warnings are essential for responsible practice.
On November 17, 2025 AT 17:15
Brandi Thompson
I have to say the article does a thorough job covering the entire spectrum of local anesthesia in oral surgery from a pharmacological standpoint to practical application and patient management it walks the reader through the chemistry behind lidocaine and articaine their lipid solubility and how that affects bone penetration and onset time then it goes on to discuss the role of epinephrine in prolonging the block while not altering the maximum dose as well as the importance of calculating dosage based on patient weight which is essential for avoiding toxicity and it emphasizes the need for slow injection technique to reduce the risk of intravascular administration and subsequent complications like tachycardia it also offers solid postoperative advice such as keeping the head elevated using soft foods and gentle saline rinses while also noting the red flag symptoms that should prompt a call to the dentist the inclusion of regulatory references like FDA and AAOMS adds credibility and guides clinicians to follow established standards overall this is a valuable resource for both new and seasoned practitioners
On November 20, 2025 AT 00:48
Chip Hutchison
Very helpful! I especially appreciated the quick checklist at the end – makes it easy to remember the key points before stepping into the operatory.
On November 22, 2025 AT 02:48
Emily Moody
Patriotic dentists should champion these anesthetic protocols; only by adhering to elite standards can we ensure the American smile stays unbeatable! 🇺🇸
On November 23, 2025 AT 23:15
Prateek Kohli
Nice guide! 👍 It’s good to see clear instructions that anyone can follow.
On November 25, 2025 AT 14:08
Noah Seidman
While the article is solid, I think it glosses over the ethical duty to discuss alternative pain‑management options beyond pharmacology.
On November 26, 2025 AT 23:28
Anastasia Petryankina
Oh, joy – another “essential guide.” As if we needed more of those. Maybe next time throw in some original research instead of rehashing textbook basics.
On November 28, 2025 AT 03:15
Tim Ferguson
Interesting take, but I’d argue that the emphasis on epinephrine may be overstated for low‑risk patients.
On November 29, 2025 AT 01:28