Erosive Esophagitis Symptom Tracker
Identify Your Triggers
Select the workplace factors that may worsen your symptoms:
Quick Relief Tactics
Select the relief methods you can use at your desk:
Workplace Meal Planning
Track your daily eating habits to reduce reflux episodes:
Symptom Management Summary
Your personalized strategy will appear here after you analyze your triggers and plan your day.
When you’re dealing with erosive esophagitis is a form of acid‑induced inflammation that erodes the lining of the esophagus, everyday office life can feel like a minefield.
Key Takeaways
- Identify common workplace triggers - posture, stress, meal timing, and certain drinks.
- Use fast‑acting on‑the‑spot tactics like proper breathing, water sips, and chewable antacids.
- Plan meals and hydration to keep stomach acid at bay without disrupting work.
- Know when and how to use prescribed medication such as proton pump inhibitors.
- Communicate clearly with managers and coworkers to create a supportive environment.
Why Symptoms flare up at the office
Most people think erosive esophagitis only hurts after a big dinner, but the office can be just as provocative. A tight‑fitting suit, long meetings, and a desk‑bound schedule all invite two main culprits: increased intra‑abdominal pressure and lowered loweresophageal sphincter (LES) tone. When you sit hunched over a laptop, your diaphragm works harder, pushing stomach contents upward. Add stress‑related cortisol spikes, and the LES - the muscular valve that keeps acid down - relaxes, letting acid splash back into the throat.
Other hidden triggers include:
- Carbonated drinks and coffee that relax the LES.
- Frequent snacking on acidic or spicy foods.
- Dehydration, which reduces saliva’s natural buffering effect.
- Standing for long periods without moving, which can increase abdominal pressure.
Fast‑acting relief you can use at your desk
When the burn starts, you need a quick fix that won’t draw unwanted attention. Here are three discreet tactics:
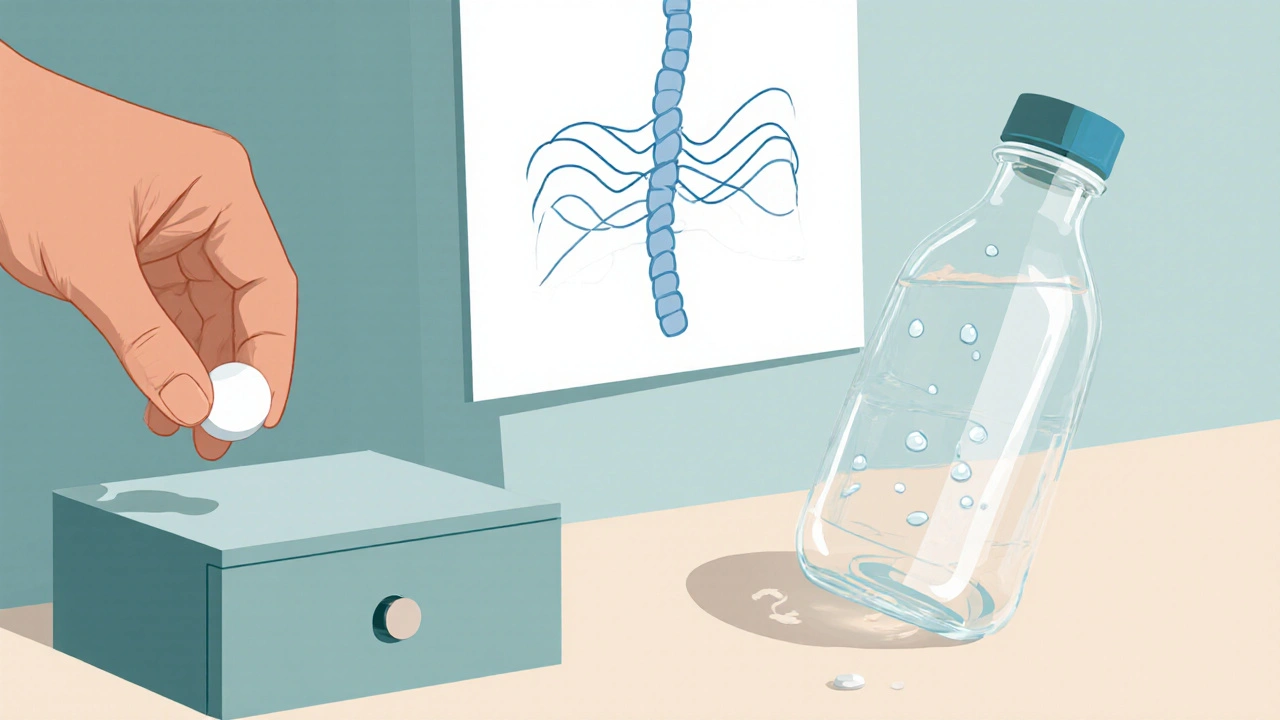
- Chewable antacid tablets: Chewing releases calcium carbonate faster than swallowing a tablet. Keep a small bottle in a drawer; a single dose can neutralize acid for up to an hour.
- Deep, diaphragmatic breathing: Inhale slowly through the nose for four counts, hold two, exhale through the mouth for six. This reduces stress hormones and gently pulls the LES upward.
- Water sip‑pause: Take a 5‑ounce sip of room‑temperature water, hold it for a few seconds, then swallow. The water buffers acid and stimulates saliva production, which contains bicarbonate that neutralizes reflux.
Meal timing and hydration tricks for the workday
Planning when and what you eat can dramatically cut symptom spikes. Aim for three main principles: smaller portions, low‑acid foods, and steady hydration.
- Eat a light breakfast that’s protein‑rich but low in fat - Greek yogurt with berries works well.
- Schedule lunch at least three hours before any critical meeting; this gives your stomach time to empty.
- Snack only on non‑citrus options like almonds or a banana. Avoid chocolate, peppermint, and tomato‑based sauces.
- Drink water throughout the day, aiming for 1.5-2L total. Use a marked bottle to track intake without breaking focus.
Remember, soda and coffee are the biggest offenders. If you need caffeine, try a short‑burst of green tea or a half‑caffeinated espresso, and always follow with a glass of water.
Medication management on a busy schedule
Most clinicians prescribe a proton pump inhibitor (PPI) for erosive esophagitis because it reduces acid production at its source. Here’s how to fit it into a typical 9‑to‑5:
- Take your PPI 30minutes before your first meal of the day - often breakfast. If you work night shifts, adjust timing to the first meal you’ll have.
- If you experience breakthrough heartburn, a short‑acting antacid (calcium carbonate or magnesium hydroxide) can be used as a rescue.
- Never double‑dose; PPIs reach full effect after 2-3 days of consistent use.
- Schedule a quarterly check‑in with your gastroenterologist to assess healing and consider stepping down medication when symptoms are under control.
Quick Relief Options at Work
| Option | How it Works | Workplace Suitability |
|---|---|---|
| Chewable Antacid | Neutralizes stomach acid quickly via calcium carbonate release. | Discrete, no water needed, effective within 5minutes. |
| Deep Breathing | Reduces stress hormones, relaxes LES. | Zero equipment, can be done at your desk. |
| Water Sip‑Pause | Buffers acid, stimulates saliva production. | Requires a water bottle; harmless to coworkers. |
| PPI (Morning Dose) | Inhibits gastric proton pumps, lowering overall acid output. | Best taken at home or before work; not a quick fix. |
| Standing Desk Adjustment | Reduces abdominal pressure by promoting better posture. | May need employer approval; benefits beyond reflux. |
Talking to your employer and coworkers
Transparency can prevent awkward moments. A brief email or chat message explaining that you have a chronic condition that benefits from occasional water breaks or sitting adjustments is usually enough. Use language like:
"I have a medical condition that can cause sudden heartburn. If I need a quick water sip or a short stretch, it won’t affect my tasks. Thanks for understanding."
Most HR policies in the UK consider this a reasonable accommodation under the Equality Act 2010. If you need a more formal adjustment-like a standing desk or a scheduled break-ask your line manager to document the request.
Ergonomic tweaks to lower pressure on your stomach
Simple workstation changes can keep the LES from working overtime:
- Raise your monitor so your screen is at eye level; this encourages an upright posture.
- Use a lumbar cushion to maintain natural spine curvature.
- Set a reminder to stand or stretch for two minutes every hour; this eases abdominal tension.
- If you can, place your keyboard slightly lower than your elbows to avoid hunching.
These tweaks not only help reflux but also reduce neck and back strain, making them a win‑win.
Long‑term lifestyle habits for lasting relief
Beyond the office, consistency is key. A handful of habits have the biggest impact:
- Weight management: Even a 5‑% reduction in body weight can lower intra‑abdominal pressure.
- Regular exercise: Low‑impact activities like walking or swimming improve digestion without jarring the stomach.
- Sleep elevation: Raising the head of your bed 6‑8inches reduces nighttime reflux, which often carries into the morning.
- Avoid tight clothing: Belt loops and skinny jeans compress the abdomen, encouraging acid back‑flow.
- Mind‑body practices: Yoga or meditation lowers cortisol, indirectly supporting LES tone.
Combine these with the workplace tactics above, and you’ll see a steady decline in flare‑ups.
Frequently Asked Questions
Can I take antacids during a meeting without drawing attention?
Yes. Chewable tablets are small, silent, and dissolve quickly. Keep a discreet container in your desk drawer and take a single dose when you feel the first hint of heartburn.
How often should I stand up to reduce reflux risk?
Aim for a brief stand‑or‑stretch break every 60 minutes. Even a two‑minute walk around the office lowers abdominal pressure and re‑sets your posture.
Is coffee a deal‑breaker for erosive esophagitis at work?
Coffee can relax the LES, but a small, low‑acid cold brew (under 5oz) paired with water often stays tolerable. If you notice symptoms after each cup, switch to green tea or herbal alternatives.
Do I need a doctor’s note to ask for a standing desk?
In the UK, a medical recommendation isn’t mandatory, but providing one speeds up the approval process. A brief note stating that a standing desk helps manage a chronic gastrointestinal condition is usually sufficient.
When should I consider stepping down from a PPI?
After at least 8-12 weeks of symptom control and an endoscopy confirming healing, discuss tapering with your gastroenterologist. Gradual reduction minimizes rebound acid production.


Comments
rachel mamuad
I love how this guide synergizes practical tips with a holistic view of workplace wellness. The typo‑prone moments are definitely relatable, like when I write “definately” in my own notes. It’s great that you’re encouraging folks to utilize posture adjustments as a low‑cost solution. The jargon‑heavy sections about LES tone are actually super useful for tech‑savvy readers. Keep sharing these kind of integrative strategies!
On October 6, 2025 AT 13:26
Amanda Anderson
I swear the burn feels like a tiny dragon doing the Macarena on my throat!
On October 14, 2025 AT 11:35
Carys Jones
Honestly, I find most of these “quick fixes” to be nothing more than corporate wellness fluff. You’re telling people to chew antacids like candy while they’re stuck in a meeting-pretty absurd. The real issue is that many employers refuse to accommodate genuine medical needs, treating us like disposable assets. It’s hypocritical to preach standing desks without addressing underlying workload pressures. If you truly care, start by advocating for systemic changes, not just individual coping tricks.
On October 22, 2025 AT 09:44
Roxanne Porter
Thank you for compiling these evidence‑based recommendations. The formal tone and clear structure make it easy to implement at work. I appreciate the emphasis on documented communication with management. These suggestions should be shared with HR departments as part of reasonable accommodation policies.
On October 30, 2025 AT 06:53
Jonathan Mbulakey
The experience of acid reflux in a modern office can be viewed as a microcosm of the tension between the body and environment. When we sit hunched over a screen, the diaphragm is forced into a suboptimal posture, which in turn increases intra‑abdominal pressure. This mechanical shift creates a cascade where the lower esophageal sphincter relaxes, allowing gastric contents to ascend. Stress hormones, particularly cortisol, further diminish sphincter tone, amplifying the problem. It is therefore not merely a dietary issue but an ergonomic and psychological one as well.
Understanding this integrated model suggests a multi‑layered approach. First, conscious posture correction realigns the thoracic cavity, reducing pressure. Second, scheduled micro‑breaks interrupt prolonged static loading, restoring circulatory flow. Third, hydration serves as a natural buffer, as water stimulates salivary bicarbonate secretion.
Moreover, the timing of meals relative to meetings respects the digestive timeline, allowing gastric emptying before cognitive demands peak. Selecting low‑acid foods minimizes the chemical load on the esophagus. In combination, these practices form a coherent strategy that honors both bodily physiology and occupational demands.
Finally, the social dimension cannot be ignored. Transparent communication with colleagues and supervisors fosters an environment where small accommodations are normalized. When we view symptom management as a collaborative project rather than an individual burden, the workplace becomes a healthier space for everyone.
On November 7, 2025 AT 05:02
Warren Neufeld
I totally get how stressful those acid flare‑ups can be at the desk. The water sip‑pause trick has helped me a lot, and it’s easy to do without anyone noticing. Also, keeping a small bottle of antacids nearby is a good idea. Hope this helps others too.
On November 15, 2025 AT 03:12
Deborah Escobedo
This guide is really helpful and positive. It gives clear steps without overwhelming the reader. The minimal punctuation makes it easy to skim. I especially like the tip about standing for two minutes each hour. Keep up the good work
On November 23, 2025 AT 01:21
Dipankar Kumar Mitra
Man, you’ve nailed the vibe of dealing with reflux at work. It’s almost philosophical-accept the burn, then act. The deep breathing thing is like a tiny meditation hack. Keep spreading these low‑key hacks, they’re gold.
On November 30, 2025 AT 23:30
Tracy Daniels
Great resource! The step‑by‑step layout makes it easy for anyone to follow. 😊 The emphasis on clear communication with managers is especially important. 👍 Looking forward to more practical health guides.
On December 8, 2025 AT 21:39
Hoyt Dawes
Honestly, this feels like a watered‑down version of a wellness retreat brochure. If you want to impress, add some cutting‑edge research or at least cite a few studies.
On December 16, 2025 AT 19:48
Jeff Ceo
I see your point, but dismissing the whole thing as fluff ignores the reality that many workers need concrete, immediate solutions. The suggestions here are actionable and low‑cost, which is exactly what busy professionals need.
On December 24, 2025 AT 17:58
David Bui
While the article is generally solid, there are a few grammatical slips that could be tightened up. For instance, “you’re” should be used instead of “your” in the section about posture. A quick proofread would improve credibility.
On January 1, 2026 AT 16:07
Alex V
Sure, because the secret to managing reflux is obviously a grand conspiracy by soda manufacturers to keep us buying fizzy drinks. They’ve been feeding us antacids while secretly installing micro‑lasers in office chairs to increase abdominal pressure. Speak up!
On January 9, 2026 AT 14:16
Robert Jackson
Nice tips but dont forget the old school method – just stand up and walk around. Sometimes that simple step beats any fancy cup of water.
On January 17, 2026 AT 12:25