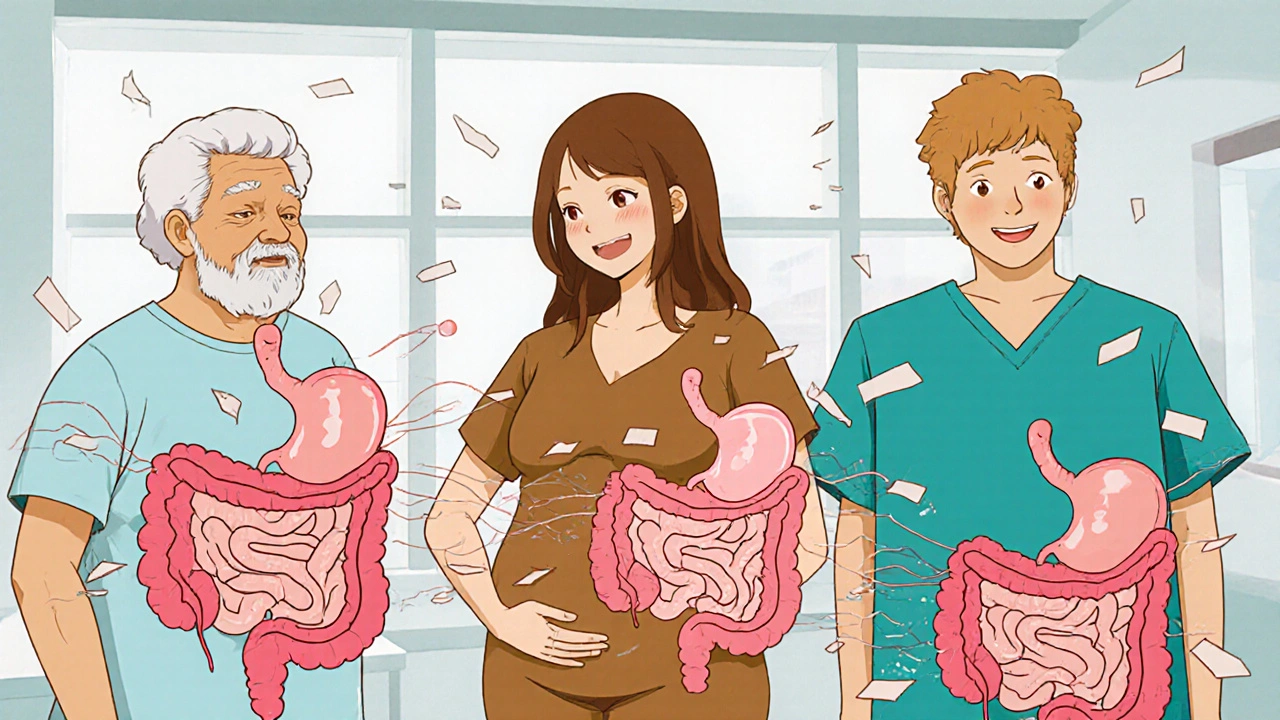
When nausea and vomiting hit hard-whether from food poisoning, chemotherapy, migraines, or even pregnancy-getting relief fast matters. Metoclopramide is one of the oldest and most commonly prescribed drugs for this exact problem. But how does it actually stop the feeling of sickness and the urge to throw up? It’s not just a pill that masks symptoms. It works deep inside your digestive system and brain, and understanding how it works helps you use it safely and effectively.
What Metoclopramide Actually Does in Your Body
Metoclopramide is classified as an antiemetic and a prokinetic agent. That means it does two things: it reduces nausea and vomiting, and it speeds up how fast your stomach empties. Most people think nausea is just a brain thing, but it’s often rooted in your gut. When food sits too long in your stomach, or when the muscles that move food along don’t work right, your body sends distress signals to your brain. That’s where the nausea kicks in.
Metoclopramide blocks dopamine receptors in two key areas: the brain’s vomiting center (in the medulla) and the gut’s nerve endings. By doing this, it cuts off the signals that tell your brain, “Something’s wrong-get ready to vomit.” At the same time, it increases contractions in the upper digestive tract. This helps food move from your stomach into your small intestine faster. Think of it like turning up the speed on a conveyor belt that’s been stuck.
For people with gastroparesis-a condition where the stomach doesn’t empty properly, often seen in diabetes-metoclopramide can be life-changing. Studies show it improves gastric emptying in up to 70% of patients after a few days of use. It’s not a cure, but it restores function where it’s broken.
How Quickly Does It Work?
If you’ve ever had severe nausea, you know time feels like it’s crawling. Metoclopramide doesn’t wait. When taken orally, you’ll usually start feeling relief within 30 to 60 minutes. If it’s given as an injection-common in hospitals or emergency rooms-the effect kicks in within 1 to 2 minutes. That’s why it’s often used in cancer centers before chemo or after surgery, when quick control of vomiting is critical.
Its effects last about 1 to 2 hours after an oral dose, which is why it’s typically taken 30 minutes before meals and at bedtime. This timing isn’t random-it’s designed to keep your stomach moving and your nausea under control when it’s most likely to flare up.
Who Uses Metoclopramide?
It’s not just for one group. People use metoclopramide for several reasons:
- Chemotherapy patients: It’s often combined with other anti-nausea drugs to handle delayed vomiting after treatment.
- People with gastroparesis: Especially those with diabetic gastroparesis, where nerve damage slows digestion.
- Migraine sufferers: Nausea is a major part of migraine attacks, and metoclopramide can help both the pain and the stomach upset.
- Pregnant women: Though not first-line, it’s sometimes used for severe morning sickness when other options fail, under strict supervision.
- Post-surgery nausea: Used in recovery rooms to prevent vomiting after anesthesia.
It’s also used off-label for acid reflux and hiccups, though these aren’t FDA-approved uses. The key is that it’s most effective when nausea is tied to slow digestion or delayed gastric emptying-not when it’s caused by inner ear issues (like motion sickness), where drugs like dimenhydrinate work better.
Side Effects You Need to Watch For
Metoclopramide isn’t risk-free. Because it affects dopamine-a brain chemical linked to movement and mood-it can cause side effects that are hard to ignore.
The most common ones are drowsiness, fatigue, and diarrhea. But the serious ones? They’re neurological. Tardive dyskinesia is a rare but permanent movement disorder that can develop after long-term use. It causes uncontrollable facial tics, lip smacking, or tongue thrusting. The risk goes up after 12 weeks of use, which is why doctors limit treatment to 4 to 12 weeks at a time.
Other neurological side effects include muscle spasms, restlessness, and even symptoms that mimic Parkinson’s disease-shakiness, stiff muscles, slow movement. These usually go away when you stop the drug, but they can be scary if you don’t know what’s happening.
That’s why metoclopramide isn’t something you should take for months on end without monitoring. If you’ve been on it for more than a few weeks and notice any odd movements or muscle tightness, talk to your doctor right away. Don’t wait.
Who Should Avoid It?
There are clear red flags for who shouldn’t take metoclopramide:
- People with a history of tardive dyskinesia or movement disorders
- Those with intestinal blockages or bleeding in the gut
- People with pheochromocytoma (a rare adrenal tumor)-metoclopramide can trigger dangerous blood pressure spikes
- Anyone allergic to the drug or similar medications
- Children under 1 year old-safety hasn’t been established
It also interacts with other drugs. Taking it with antidepressants like SSRIs or MAOIs can increase the risk of serotonin syndrome-a potentially life-threatening condition. Mixing it with antipsychotics or other dopamine blockers can make movement side effects worse. Always tell your doctor what else you’re taking, even over-the-counter meds or supplements.
How It Compares to Other Anti-Nausea Drugs
| Medication | Best For | Onset of Action | Duration | Key Risk |
|---|---|---|---|---|
| Metoclopramide | Stomach-related nausea, gastroparesis, post-op vomiting | 30-60 min (oral), 1-2 min (injection) | 1-2 hours | Tardive dyskinesia with long-term use |
| Ondansetron (Zofran) | Chemotherapy-induced nausea, severe vomiting | 30 min | 4-8 hours | Headache, constipation, rare heart rhythm issues |
| Diphenhydramine (Benadryl) | Motion sickness, vertigo | 15-30 min | 4-6 hours | Drowsiness, dry mouth, confusion in older adults |
| Promethazine (Phenergan) | Motion sickness, post-op nausea | 20 min | 4-6 hours | Sedation, risk of tissue damage if injected incorrectly |
| Dimenhydrinate (Dramamine) | Travel sickness, mild nausea | 15-30 min | 4-6 hours | Drowsiness, dizziness |
Metoclopramide stands out because it doesn’t just block nausea signals-it fixes the underlying cause by moving food along. That’s why it’s preferred for gastroparesis. But if your nausea is from inner ear problems or severe chemo, other drugs like ondansetron may be more effective and safer for long-term use.
How to Take It Safely
If your doctor prescribes metoclopramide, follow these steps:
- Take it 30 minutes before meals and at bedtime-this timing matches your stomach’s natural rhythm.
- Don’t crush or chew extended-release tablets. Swallow them whole.
- Use the lowest dose possible. For adults, the standard is 10 mg, 3-4 times daily. Never exceed 40 mg per day.
- Set a reminder to stop after 12 weeks unless your doctor says otherwise.
- Watch for muscle stiffness, twitching, or unusual movements. Report them immediately.
- Don’t drink alcohol. It makes drowsiness and dizziness worse.
Store it at room temperature, away from moisture. Keep it out of reach of children. If you miss a dose, take it as soon as you remember-but skip it if it’s almost time for the next one. Never double up.
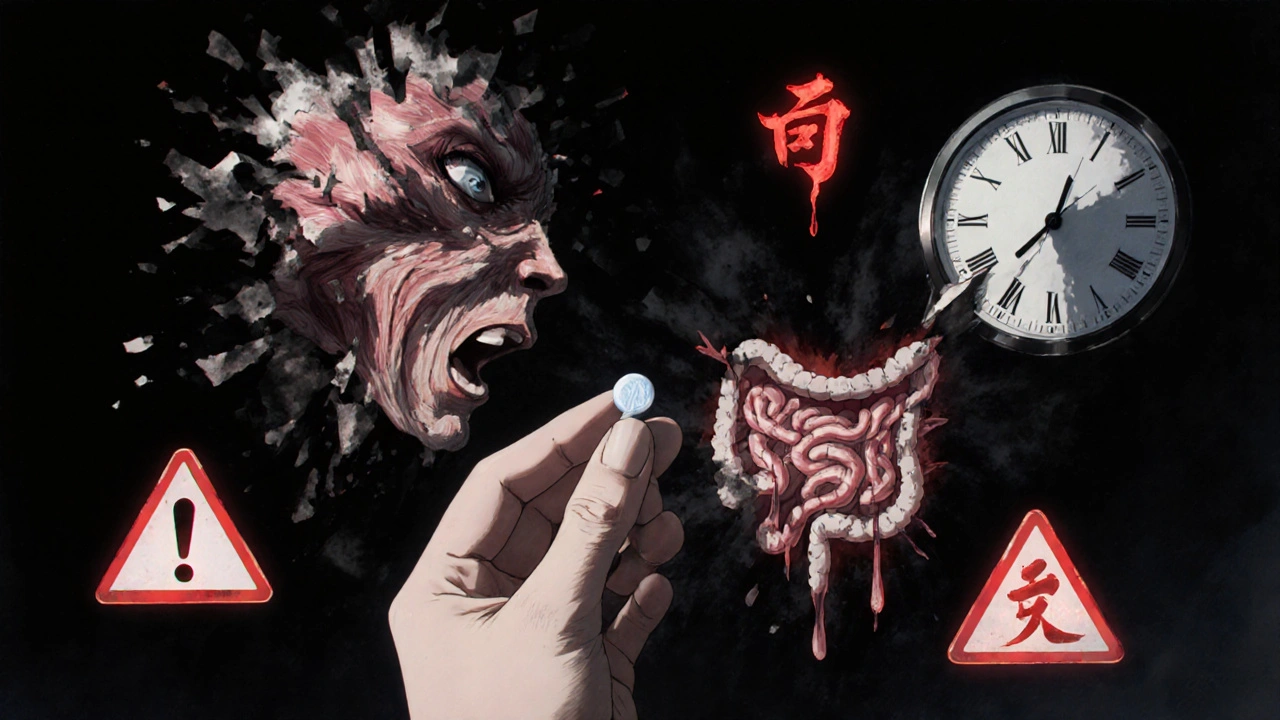
When to Call Your Doctor
Metoclopramide is generally safe for short-term use. But you should call your doctor right away if you experience:
- Involuntary movements of your face, tongue, or limbs
- High fever, stiff muscles, confusion, or rapid heartbeat-signs of neuroleptic malignant syndrome (rare but serious)
- Severe dizziness or fainting
- Signs of an allergic reaction: rash, swelling, trouble breathing
These are rare, but they’re emergencies. Don’t wait.
Final Thoughts: Is Metoclopramide Right for You?
Metoclopramide works well when nausea comes from a slow or stuck digestive system. It’s not a magic bullet for all types of vomiting, and it’s not meant for long-term use. But for people with gastroparesis, post-op nausea, or chemo-related vomiting, it’s a proven tool that gets results.
The key is using it the right way: short-term, at the right dose, with awareness of the risks. If you’ve been struggling with nausea that won’t quit, talk to your doctor about whether metoclopramide fits your situation. Don’t assume it’s safe just because it’s been around for decades. Your body’s response matters more than its history.
Can metoclopramide be used for morning sickness during pregnancy?
Yes, but only under a doctor’s supervision. While it’s not the first choice for morning sickness, studies show it can be effective and safe in the second and third trimesters when other treatments fail. The risk of birth defects is low, but doctors usually try safer options like vitamin B6 or doxylamine first. Long-term use is avoided during pregnancy.
How long does metoclopramide stay in your system?
Metoclopramide has a half-life of about 5 to 6 hours in healthy adults. That means half the drug leaves your body in that time. After 24 to 36 hours, almost all of it is cleared. But in people with kidney problems, it can build up, which increases side effect risks. Dose adjustments are needed for those with reduced kidney function.
Is metoclopramide addictive?
No, metoclopramide is not addictive. It doesn’t produce euphoria or cravings like opioids or benzodiazepines. However, some people may feel they need it because their nausea returns when they stop. This isn’t addiction-it’s a sign their underlying condition (like gastroparesis) still needs treatment. Always taper off under medical guidance.
Can you take metoclopramide with food?
It’s best taken on an empty stomach, 30 minutes before meals. Taking it with food can delay absorption and reduce its effectiveness. If you’re nauseated and can’t keep anything down, your doctor might suggest an injection instead.
What happens if I stop metoclopramide suddenly?
Stopping suddenly won’t cause withdrawal symptoms like with some other drugs. But your nausea and vomiting may return quickly, especially if you’re using it for a chronic condition like gastroparesis. Your doctor may recommend tapering the dose gradually to avoid rebound symptoms.
Is there a generic version of metoclopramide?
Yes, metoclopramide is available as a generic drug in tablets, oral syrup, and injectable forms. It’s significantly cheaper than brand-name versions like Reglan. Generic metoclopramide is just as effective and widely prescribed. Always check with your pharmacist to confirm you’re getting the generic version unless your doctor specifies otherwise.
Next Steps If You’re Considering Metoclopramide
If you’re thinking about using metoclopramide, start by tracking your symptoms. Note when nausea happens, what triggers it, and how long it lasts. Bring this log to your doctor. Ask: “Is my nausea likely caused by slow stomach emptying?” If the answer is yes, metoclopramide might help. If not, there are better options.
Don’t self-prescribe. Even though it’s available by prescription only, some people try to get it from friends or online sources. That’s dangerous. Side effects can be serious, and it interacts with many common medications. Always get it through a licensed provider who can monitor your response.
For many, metoclopramide is the difference between feeling sick all day and being able to eat, work, or enjoy time with family. Used wisely, it’s a powerful tool. Used carelessly, it can cause harm. Know your body. Know the risks. And never ignore warning signs.


Comments
Manuel Gonzalez
Metoclopramide saved my life after chemo. I was throwing up every 20 minutes until my oncologist prescribed it. Within an hour, I could actually sit up and drink water. Not magic, just science working right.
Don't let the side effect warnings scare you off if you're under supervision. I've been on it for 8 weeks now and no tics. Just a quiet, functioning digestive system.
On November 1, 2025 AT 03:43
Brittney Lopez
I'm a nurse and I've seen this drug turn people around. One patient with diabetic gastroparesis hadn't eaten a real meal in three months. After two days on metoclopramide? She cried because she could smell her daughter's cooking without wanting to puke.
It's not perfect, but sometimes 'good enough' is everything.
On November 2, 2025 AT 22:56
Jens Petersen
Let’s be honest-this is just dopamine suppression dressed up as medicine. You’re not fixing the gut; you’re silencing the alarm system. It’s like putting duct tape over a smoke detector because you don’t like the noise.
And yet, people treat it like some miracle cure. Pathetic. The real issue? Pharma’s obsession with Band-Aid solutions instead of root-cause healing. Also, anyone who takes this longer than 4 weeks is either delusional or has a doctor who doesn’t read the FDA label. Which is worse?
On November 4, 2025 AT 15:40
Keerthi Kumar
In India, we call this 'the quiet warrior'-it doesn’t shout, but it fights deep inside. My grandmother had gastroparesis after her diabetes diagnosis; she couldn’t even keep rice down. We tried ginger, ayurveda, acupuncture-nothing worked. Then, after months of despair, her doctor gave her metoclopramide. She ate her first proper meal in a year-and wept.
Modern medicine isn’t the enemy of tradition; sometimes, it’s the bridge.
But yes, please, please, please-don’t use it beyond 12 weeks. The body remembers, and so do the nerves.
On November 4, 2025 AT 16:36
Dade Hughston
so i took this for like 3 weeks after my surgery and yeah it worked but then i started getting this weird twitch in my cheek like every 5 minutes and i was like oh shit is this the thing they warn about and i just stopped it cold turkey and now i feel fine but like why do they even make this if it can do that and also i think my doctor just wanted to get me out of his office fast
also why is it called metoclopramide like who named this and why does it sound like a robot sneezing
On November 6, 2025 AT 03:05
Jim Peddle
Interesting how this drug is pushed so aggressively for pregnancy nausea while barely any long-term fetal studies exist. And yet, the FDA allows it. Coincidence? Or is this another case of Big Pharma exploiting desperation?
Also, notice how they mention 'off-label' uses like hiccups and reflux-classic tactic. Get people hooked on the side effects, then pivot to 'off-label' as if it’s a loophole. Meanwhile, the dopamine blockade is still happening. No one talks about the long-term neurochemical rewiring. They just say 'it’s safe if used short-term.' Safe for whom? The patient? Or the stock price?
On November 7, 2025 AT 01:06
S Love
If you’re considering metoclopramide, here’s the real advice: track your symptoms before you start. Write down what triggers your nausea, how bad it gets, and how long it lasts.
Then, when you’re on it, track again. Did your meals become easier? Did the vomiting stop? Did you start sleeping through the night?
This isn’t just about taking a pill-it’s about reclaiming your life. And if you notice any weird movements? Don’t wait. Call your doctor that day. Better safe than sorry.
You’ve got this.
On November 7, 2025 AT 06:43
Pritesh Mehta
Western medicine is obsessed with chemical fixes while ignoring the ancient wisdom of India and China where food is medicine and digestion is sacred. Metoclopramide? A crude hammer for a delicate clock. We have herbs like ginger, fennel, and triphala that gently stimulate motility without poisoning the nervous system. Why do you think Indian mothers give children boiled cumin water for upset stomachs? Because they’ve known for centuries: the gut is the soul’s first temple.
And yet, here we are, trusting a synthetic dopamine blocker over millennia of empirical knowledge. Progress? Or cultural surrender?
On November 8, 2025 AT 23:41
Billy Tiger
Who the hell lets a drug like this be prescribed for pregnancy? That’s just asking for trouble. You think they care about your baby? Nah. They care about the lawsuit if you don’t take it and the baby comes out weird. So they push it. Then when the kid grows up with tics? They blame genetics.
Also why is this even legal? It’s basically a chemical restraint. You’re not healing-you’re suppressing. And if you’re not on it long enough to get tardive dyskinesia? Congrats. You’re just a guinea pig with a prescription.
On November 10, 2025 AT 18:23
Katie Ring
Metoclopramide isn’t a cure-it’s a compromise. We’ve turned our bodies into machines that need software patches. We don’t fix the broken digestive rhythm. We jam a neurochemical wrench into it and call it progress.
And yet… I took it. I needed it. I didn’t want to die of dehydration from vomiting for the third day straight. So I chose survival over purity. Is that weakness? Or just being human in a world that offers no better options?
Maybe the real tragedy isn’t the drug. It’s that we need it at all.
On November 10, 2025 AT 21:43
Adarsha Foundation
Thank you for writing this with such care. I’ve seen too many people scared away by the side effects without understanding the context. For some, this drug is the only thing standing between them and hospitalization.
Let’s not demonize it. Let’s not glorify it. Let’s just use it wisely-with awareness, with monitoring, with compassion.
And if you’re reading this and you’re on it? You’re not alone. We’re all just trying to feel human again.
On November 11, 2025 AT 08:47
Alex Sherman
It’s funny how people treat metoclopramide like some forgotten relic of 1970s pharmacology. But here’s the truth: it’s one of the few drugs that actually targets the *mechanism* of nausea-not just the symptom. Most antiemetics are like putting a blanket over a fire. This? This is turning off the gas.
And yes, the side effects are real. But so is the suffering of someone who can’t keep water down for days.
Stop pretending medicine is perfect. It’s messy. It’s imperfect. But sometimes, imperfect is the only thing standing between you and death.
On November 12, 2025 AT 15:20