What is neuropathic pain?
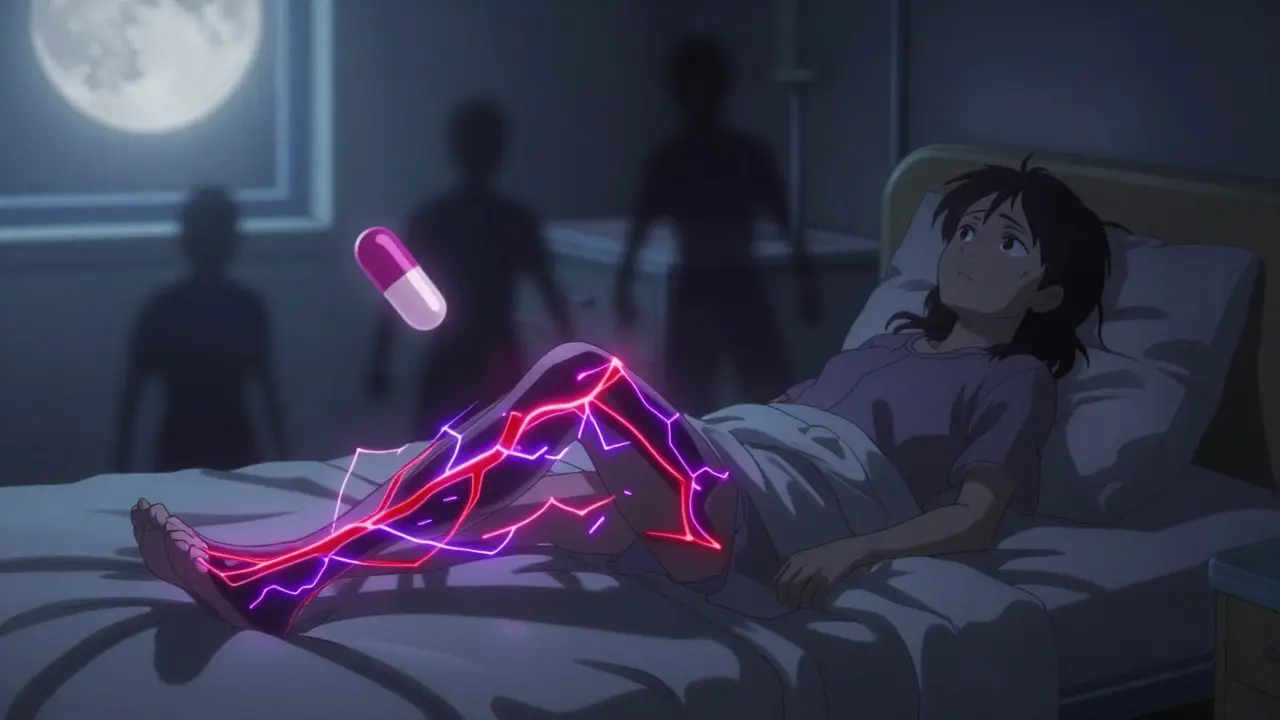
Neuropathic pain isn’t the kind of pain you feel after stubbing your toe or pulling a muscle. It’s caused by damaged or malfunctioning nerves sending wrong signals to your brain. People describe it as burning, shooting, or like electric shocks. Some feel tingling or numbness, even when nothing’s touching their skin. This isn’t just discomfort-it can make everyday life unbearable. Simple things like wearing socks or lying in bed can trigger sharp pain. Around 7 to 10% of adults deal with this kind of pain, and diabetes is the biggest cause, responsible for about 30% of cases.
Unlike regular pain that fades as an injury heals, neuropathic pain sticks around. It doesn’t respond well to regular painkillers like ibuprofen or even opioids. That’s why doctors turn to medications originally made for seizures and depression. Two of the most common are gabapentin and pregabalin. They’re not cures, but they help many people get back some control over their lives.
How gabapentin and pregabalin work
Both gabapentin and pregabalin are chemically similar to GABA, a calming brain chemical. But they don’t work like GABA. Instead, they latch onto a specific part of nerve cells called the alpha-2-delta subunit. This part controls how much calcium flows into nerves. Too much calcium means nerves fire too easily, sending pain signals even when there’s no injury. By blocking this, these drugs quiet down the overactive nerves.
The big difference? Pregabalin binds to that target about six times more tightly than gabapentin. That means it works more efficiently. Gabapentin’s absorption is messy-it doesn’t always get absorbed the same way depending on how much you take or what you ate. Pregabalin? It’s consistent. Whether you take it on an empty stomach or after a meal, your body gets the same amount. That predictability matters when you’re trying to find the right dose.
Dosing: Simple vs. complicated
Gabapentin’s dosing is a headache for many. Because it doesn’t last long-only 5 to 7 hours-you have to take it three times a day. Starting low is key. Doctors usually begin with 100 to 300 mg at night to avoid dizziness. Then, every few days, they bump it up by 100 to 300 mg. It can take weeks to reach the full dose of 3,600 mg per day. Many people give up because it’s too hard to remember three doses a day, or they get too dizzy too fast.
Pregabalin is simpler. You start at 75 mg once or twice a day. Most people reach their effective dose in under two weeks. The max is usually 300 to 600 mg per day, split into two doses. That’s easier to stick with. A 2023 clinical trial found patients reached their target dose in just over 8 days with pregabalin, compared to nearly 15 days with gabapentin.
Effectiveness: Who gets relief?
Neither drug works for everyone. About 30% of people on gabapentin get at least half their pain relief. For pregabalin, that number is closer to 35%. That might not sound like a big gap, but in pain management, even 5% matters. In head-to-head studies, 68% of pregabalin users hit the 50% pain reduction mark at 12 weeks, compared to 59% for gabapentin.
One Reddit user, u/NeuropathyWarrior, wrote: “Pregabalin knocked my pain from 8/10 to 3/10 in 48 hours-but I gained 12 lbs in six weeks.” Another said: “Gabapentin made me dizzy and I fell twice. Switched to pregabalin and felt better at half the dose.”
But effectiveness isn’t just about numbers. Some people respond better to one than the other. It’s not about which is “better”-it’s about which fits you. If you need fast relief and can handle side effects, pregabalin might be the pick. If you’ve tried it before and it didn’t work-or you’re worried about weight gain-gabapentin is still a solid option.

Side effects: What to expect
Both drugs cause dizziness, sleepiness, and swelling in the legs. But pregabalin has higher rates of these. About 32% of people on pregabalin feel dizzy, compared to 26% on gabapentin. Somnolence hits 23% vs. 19%. And then there’s weight gain.
That’s where pregabalin really stands out-and not in a good way. Around 12% of users gain 5 to 15 pounds in the first month. Gabapentin? Only 3% do. For someone already struggling with mobility or diabetes, that extra weight can make pain worse. PatientsLikeMe data shows pregabalin scores 4.8 out of 10 for tolerability. Gabapentin scores 5.9.
Both can cause swelling, confusion, or even rare but serious reactions like angioedema (swelling of the face or throat). The FDA added black box warnings for both in 2008 because of increased suicidal thoughts. That’s rare-0.4% vs. 0.2% in placebo groups-but it’s real. Never stop these drugs suddenly. It can trigger seizures.
Cost and access
Gabapentin is cheap. Generic versions cost around $15 for 90 capsules of 300 mg. Most insurance plans, including Medicare, cover it. That’s why rural clinics and safety-net hospitals use it more often. Pregabalin? Generic versions are about $28 for 60 capsules of 75 mg. That’s still affordable, but it’s almost double the price. And because pregabalin is a Schedule V controlled substance (since 2019), some pharmacies require extra paperwork or limit refills.
That control status was added because of misuse. There were 12.3 overdose deaths linked to pregabalin in 2023. Gabapentin? Zero. That doesn’t mean gabapentin is safe to abuse-it’s not-but pregabalin has a higher risk profile.
Who gets which drug?
Guidelines from the American Diabetes Association recommend pregabalin as first-line for diabetic nerve pain. Why? Because its effects are more predictable, and studies show it works better in this group. But the Neuropathic Pain Special Interest Group still lists both as first-line, saying the choice should be personal.
Doctors in academic centers and big cities tend to start with pregabalin. In rural areas or clinics serving low-income patients, gabapentin is the default. One 2024 study found 68% of safety-net hospitals prescribe gabapentin first. In university hospitals? It’s 57% pregabalin.
If you’re on a tight budget, gabapentin wins. If you struggle with remembering doses, pregabalin’s twice-daily schedule is easier. If weight gain is a concern-especially if you have diabetes or heart issues-gabapentin is safer. If you need fast relief and can handle side effects, pregabalin might be worth the trade-off.

What if neither works?
These drugs aren’t magic. About 40% of people don’t get enough relief from either. That’s why doctors often combine them with other treatments. Duloxetine (Cymbalta) is another first-line option, especially if you also have depression. Topical lidocaine patches help for localized pain. Some people benefit from physical therapy, acupuncture, or nerve blocks. Newer drugs like cenobamate are showing promise, but they’re not widely used yet.
Don’t give up if one drug fails. Try the other. Or combine it with a low-dose antidepressant. Pain management is rarely one-size-fits-all. It’s trial, error, and patience.
Long-term outlook
Gabapentin isn’t going away. It’s too cheap, too widely available, and too well-studied. Even with its quirks, it’s still the go-to for millions. Pregabalin’s market share is slowly shrinking as newer drugs arrive. But it’s still the faster, more reliable option for many.
Experts agree: the goal isn’t to pick the “best” drug. It’s to find the one that gives you the most relief with the least trouble. For some, that’s gabapentin. For others, it’s pregabalin. For a few, it’s both-or neither. The right choice depends on your body, your life, and your priorities.
Can gabapentin and pregabalin be taken together?
Doctors rarely prescribe gabapentin and pregabalin together because they work the same way. Taking both doesn’t usually improve pain relief but doubles the risk of side effects like dizziness, swelling, and drowsiness. There’s no strong evidence that combining them is better than using one at a full dose. If one drug isn’t working, switching to the other is preferred over combining them.
How long does it take for pregabalin or gabapentin to work?
Some people feel better in 2 to 3 days with pregabalin, especially if they’re sensitive to the drug. Gabapentin usually takes longer-1 to 3 weeks-to reach full effect. That’s because it needs time to build up in your system, and doctors start low to avoid side effects. Don’t expect instant relief. Patience and consistent dosing matter more than speed.
Do these drugs cause addiction?
Neither drug is addictive in the way opioids are. But pregabalin is classified as a Schedule V controlled substance because some people misuse it for its calming or euphoric effects, especially when combined with alcohol or other drugs. Gabapentin has very low abuse potential. Still, both can cause physical dependence. Stopping suddenly can lead to anxiety, insomnia, nausea, or even seizures. Always taper off under medical supervision.
Can I drink alcohol while taking gabapentin or pregabalin?
No. Alcohol makes dizziness, drowsiness, and coordination problems much worse. It can also increase the risk of falls, especially in older adults. Even one drink can be dangerous when combined with either drug. Most doctors strongly advise avoiding alcohol entirely while on these medications.
What happens if I miss a dose?
If you miss a dose of gabapentin, take it as soon as you remember-but only if it’s not close to your next dose. Don’t double up. For pregabalin, same rule applies. Missing doses can cause your pain to return or make withdrawal symptoms more likely. If you often forget, use pill organizers or phone reminders. Consistency is key for both drugs to work.
Are there natural alternatives to these drugs?
Some people try supplements like alpha-lipoic acid, curcumin, or CBD oil. A few small studies show alpha-lipoic acid may help diabetic nerve pain, but the evidence isn’t strong enough to replace medication. CBD has limited data and isn’t regulated. Physical therapy, yoga, and acupuncture can help manage symptoms but rarely replace drug therapy. Don’t stop your prescribed meds without talking to your doctor-uncontrolled neuropathic pain can get worse over time.
Final thoughts
Neuropathic pain is exhausting. It doesn’t show up on X-rays or blood tests. It doesn’t go away with rest. But it can be managed. Gabapentin and pregabalin aren’t perfect, but they’re tools-effective for many, flawed for some. The goal isn’t to eliminate pain completely. It’s to reduce it enough that you can sleep, walk, and live without fear. If one drug doesn’t work, try the other. Talk to your doctor about side effects. Adjust your expectations. And remember: you’re not alone. Millions are walking this path, and there’s a way forward-even if it’s slow.

Comments
Stephen Craig
It's wild how two drugs that work the same way can feel so different in real life. One's a slow burn, the other hits like a freight train. Neither fixes you, but they let you breathe again.
On January 5, 2026 AT 02:48
Charlotte N
I tried gabapentin for six months... it made me feel like a zombie who forgot how to walk... then switched to pregabalin and my pain dropped... but now I'm 15 pounds heavier and my socks feel like sandpaper... I don't know what to do anymore
On January 6, 2026 AT 22:08
Uzoamaka Nwankpa
I wish people would stop acting like these drugs are the answer. They're just bandages on a broken bone. No one talks about the real issue: why are we medicating pain instead of fixing the root cause?
On January 7, 2026 AT 19:42
Michael Rudge
Of course the pharmaceutical companies love pregabalin. Six times tighter binding? That's not science, that's a marketing slogan wrapped in a patent. Gabapentin's been around since the 90s. They just needed a newer, pricier version to keep the cash flowing.
On January 8, 2026 AT 04:04
Angie Rehe
You people act like gabapentin is some miracle drug because it's cheap. That's not healthcare, that's rationing. If your insurance won't cover pregabalin, your doctor isn't trying hard enough. You're not saving money-you're sacrificing quality of life.
On January 9, 2026 AT 11:46
Doreen Pachificus
I've been on both. Gabapentin made me sleepy but I could still work. Pregabalin made me feel like I was underwater. I stuck with gabapentin. Not because it's better, just because I didn't feel like I was drowning in my own body.
On January 10, 2026 AT 10:40
Abhishek Mondal
Let me clarify something: the fact that pregabalin binds six times more tightly to the alpha-2-delta subunit is not a pharmacological advantage-it's a consequence of molecular optimization. The real issue is the pharmacokinetic profile, which is why you see greater inter-individual variability with gabapentin due to saturable transport mechanisms in the small intestine.
On January 11, 2026 AT 07:52
en Max
The clinical data is clear: pregabalin demonstrates superior efficacy in diabetic neuropathic pain cohorts, with statistically significant improvements in NRS scores at 12 weeks (p<0.01). However, the trade-off in tolerability-particularly weight gain and somnolence-requires careful risk-benefit analysis, especially in patients with metabolic syndrome.
On January 13, 2026 AT 00:00
Ethan Purser
I've been on both. Pregabalin gave me my life back for three months. Then I gained 20 pounds. My knees gave out. My wife left me. I switched back to gabapentin. I'm slower, I'm tired, but I'm alive. And I can still hug my dog without crying from the pain. That's the real win.
On January 13, 2026 AT 12:46
josh plum
The government made pregabalin a controlled substance because they know it's being used to get high. People are mixing it with opioids and drinking alcohol until they pass out. And you're sitting here talking about dosing schedules like it's a yoga class? Wake up.
On January 14, 2026 AT 02:16
Jack Wernet
While it is true that pregabalin offers greater bioavailability and more consistent pharmacokinetics, one must also consider the socioeconomic context in which these medications are prescribed. In underserved communities, cost and accessibility often override clinical preference, a reality that must be acknowledged without judgment.
On January 14, 2026 AT 14:14
Ashley Viñas
Honestly, if you're still taking gabapentin because it's cheap, you're not being frugal-you're being exploited. Your doctor isn't choosing for you, they're choosing for the system. You deserve better than a drug that makes you dizzy just because it's on a formulary.
On January 16, 2026 AT 09:05
Chris Cantey
It's not about which drug works better. It's about which one lets you keep your dignity. Gabapentin makes you feel like you're walking through molasses. Pregabalin makes you feel like you're melting. Neither is freedom. But one is less humiliating.
On January 17, 2026 AT 19:06
Brendan F. Cochran
i got pregabalin and it was a game changer untill i gained 30 lbs and my dr said oh thats normal. normal?? i cant even tie my shoes now. gabapentin made me sleepy but at least i could still move. so i went back. no regrets.
On January 18, 2026 AT 16:53
John Ross
The real tragedy isn't the side effects-it's that we treat neuropathic pain like a pharmacological puzzle instead of a neurological condition. We need more research into neuroplasticity, neuromodulation, and non-pharmacological interventions. Drugs are stopgaps, not solutions.
On January 20, 2026 AT 15:03