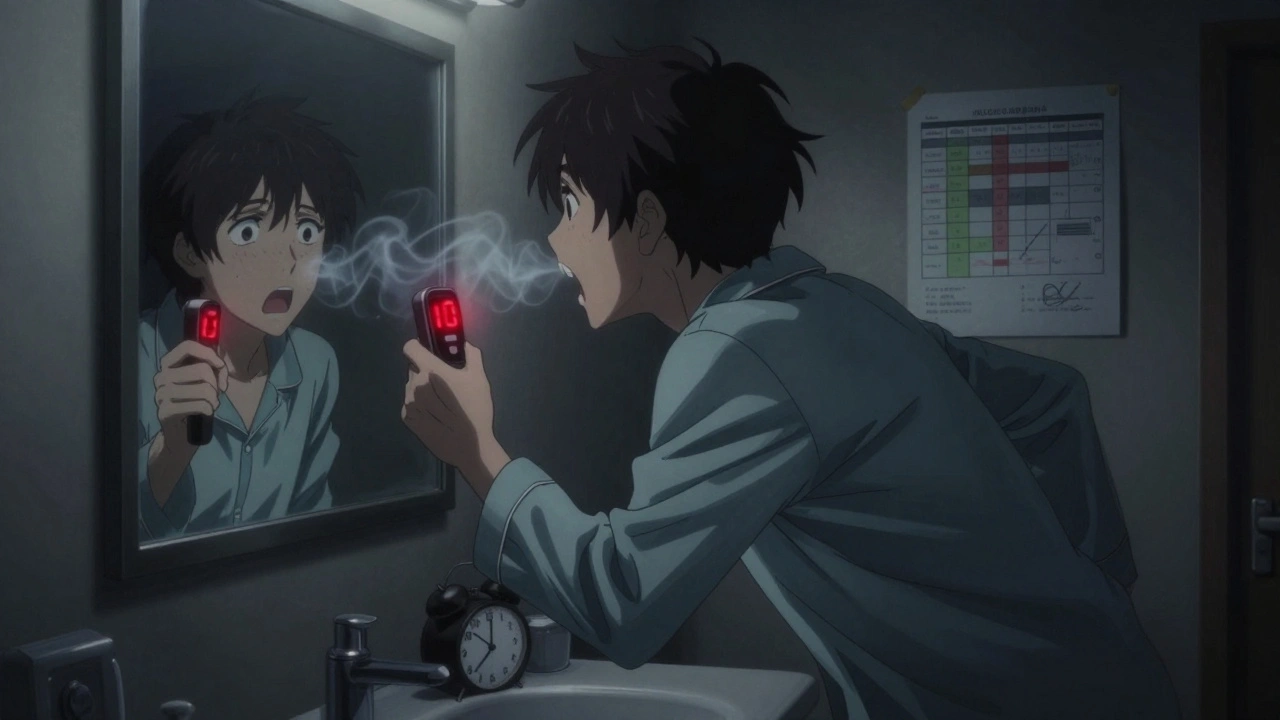
When your asthma is under control, you might not think much about your breathing. But on bad days-or even before you feel symptoms-it’s easy to miss the warning signs. That’s where peak flow monitoring comes in. It’s not fancy, it doesn’t need a doctor’s office, and it can give you a heads-up hours or even days before you start wheezing or coughing. All you need is a small hand-held device, a notebook or phone app, and a consistent routine.
What Is Peak Flow Monitoring?
Peak expiratory flow (PEF) measures how fast you can blow air out of your lungs after taking a deep breath. It’s a simple number-measured in liters per minute-that tells you how open your airways are right now. Think of it like checking your car’s oil level before a long drive. You don’t wait until the engine seizes to look under the hood.
This tool has been around since the 1950s, but it’s still a key part of asthma management today. The Global Initiative for Asthma (GINA) guidelines from 2023 say peak flow meters are especially useful when spirometry-the gold-standard lung test-isn’t available. For people who don’t notice their symptoms until they’re in trouble, peak flow readings can be the only early warning system they have.
Why Daily Tracking Matters
You can’t trust a single reading. Lung function changes naturally throughout the day. Most people have their lowest peak flow numbers right after waking up-sometimes 15% to 20% lower than in the afternoon. That’s normal. What matters is spotting changes from your usual pattern.
Doctors recommend taking two readings every day: once in the morning (between 7 and 9 a.m.) and once in the evening (between 6 and 8 p.m.). Do it at the same time, every day. Skip days, and you lose the ability to spot trends. A drop from 400 to 320 might not sound like much-but if your personal best is 450, that’s a 17% drop. That’s a red flag.
Studies show that peak flow can fall 24 to 48 hours before you feel any asthma symptoms. If you only check when you’re wheezing, you’re already behind. Daily tracking turns guesswork into action.
How to Find Your Personal Best
Your personal best isn’t what the chart on the meter says. It’s not based on your age, height, or gender. It’s the highest number you can consistently blow out when your asthma is under control.
To find it, take your peak flow reading twice a day for two to three weeks. Do it when you feel fine-no coughing, no shortness of breath, no rescue inhaler use. Record the highest number from each session. After 14 to 21 days, the highest of all those numbers is your personal best.
Some experts suggest recording readings before and after using your quick-relief inhaler during this time. That helps you see how much your meds help. For kids, this number changes as they grow. Recheck it every six to twelve months.
Important: Use the same peak flow meter every single time. Different brands give different readings. If you switch meters, your personal best becomes meaningless.
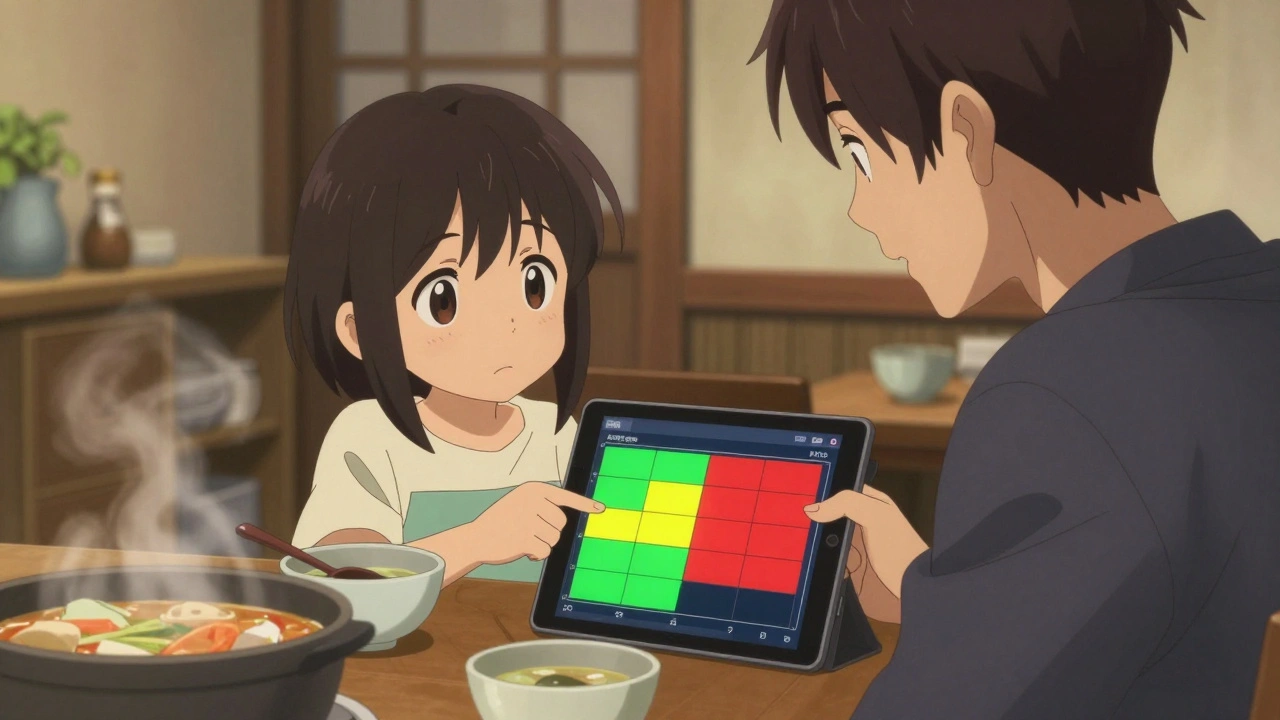
The Three Zones: Your Asthma Action Plan
Once you know your personal best, divide your readings into three zones-green, yellow, and red. These aren’t arbitrary. They’re based on percentages of your personal best and tell you exactly what to do.
- Green Zone (80%-100% of personal best): You’re in control. Keep taking your daily medications. No changes needed.
- Yellow Zone (50%-79% of personal best): Warning. Your airways are narrowing. This is the time to act-before you’re in trouble. A drop of 20% to 30% from your personal best often means an asthma episode is starting. Follow your action plan: increase your controller inhaler, avoid triggers, and monitor closely.
- Red Zone (below 50% of personal best): Medical alert. Your airways are severely restricted. Use your rescue inhaler immediately. Call your doctor or go to the ER. Don’t wait. This is when people end up in the hospital.
The American Lung Association and the Asthma and Allergy Foundation of America both use this traffic-light system. It’s simple. It’s proven. And it saves lives.
How Often Should You Measure?
It depends on your asthma. If your asthma is mild and stable, checking two or three times a week might be enough. But if you’ve had recent flare-ups, take daily meds, or have moderate to severe asthma, you need to measure twice a day-every day.
The Severe Asthma Toolkit recommends at least eight weeks of daily tracking to understand your true pattern. Even if you feel fine, keep going. Patterns take time to emerge. A single bad day doesn’t mean your treatment isn’t working. But a steady drop over three days? That’s a signal.
Some people only measure when they feel off. That’s risky. By then, it’s often too late. The goal isn’t to react to symptoms-it’s to prevent them.
Pro Tips for Accurate Readings
Peak flow meters are simple-but only if you use them right. Here’s how to get the most accurate numbers:
- Stand up straight or sit up tall. Don’t slouch.
- Take the deepest breath you can.
- Seal your lips tightly around the mouthpiece.
- Blow out as hard and fast as you can-like you’re blowing out birthday candles.
- Do it three times. Write down the highest number. Don’t average them.
- Wait 15 seconds between tries. Rest if you need to.
- Record the number, time, and any symptoms or triggers right away.
Some people get inconsistent readings because they don’t blow hard enough. If your three numbers vary by more than 20%, you’re not giving your best effort. Practice with your doctor or nurse until you get it right.
What If Your Numbers Don’t Match How You Feel?
That happens. Sometimes you feel fine but your peak flow is dropping. Other times, you feel awful but the number looks okay. Neither means you’re doing it wrong.
If your peak flow is low but you feel okay, you might be one of those people who don’t notice symptoms until it’s serious. That’s why tracking matters. Don’t ignore the number.
If your peak flow is normal but you’re wheezing or coughing, your airways might be blocked in a way that doesn’t show up on the meter. That’s rare, but it happens. Trust your body too. Use your rescue inhaler. Call your doctor. Numbers guide you-they don’t replace your instincts.
When to See Your Doctor
Don’t wait for a red zone to call. If your peak flow drops below 80% of your personal best for more than two days in a row, even if you’re in the yellow zone, talk to your doctor. Your controller meds might need adjusting.
Also, if your personal best changes by more than 10% over a few weeks without a clear reason, get it checked. That could mean your asthma is worsening-or your meter is broken.
Bring your peak flow meter to every appointment. Your doctor needs to see the actual device you’re using, not just the numbers. They’ll check if it’s calibrated right and if you’re using it correctly.
What About Apps and Digital Trackers?
Yes, you can use your phone. Many peak flow meters now connect to apps that store your readings, show trends, and even send alerts. But don’t rely on the app alone. You still need to take the measurement the same way every time.
Some people find digital trackers easier because they automatically log the date and time. Others prefer paper diaries because they’re always there and don’t need charging. Pick what works for you. The goal isn’t the tool-it’s the consistency.
Limitations and What’s Next
Peak flow monitoring isn’t perfect. It doesn’t measure everything. It can’t detect inflammation in your lungs, only how wide your airways are. Spirometry is more accurate and gives more detailed info. But not everyone has access to it. For most people with asthma, especially those managing it at home, peak flow is the most practical, affordable, and effective tool they have.
The American Thoracic Society says spirometry is preferred when available-but peak flow remains essential for daily self-management. It’s not a replacement. It’s a companion.
And for people who’ve had severe asthma attacks in the past, it’s often the difference between staying home and ending up in the ER.
Start Today
You don’t need to be perfect. You just need to be consistent. Pick a time in the morning and a time at night. Get a meter. Write down the numbers. Find your personal best. Set your zones. Stick with it.
Peak flow monitoring isn’t about fear. It’s about control. It’s about knowing your body better than anyone else can. And when you catch a problem early, you don’t just avoid an attack-you avoid the stress, the missed work, the hospital visits, and the fear that comes with it.
Start today. Your lungs will thank you tomorrow.
How often should I check my peak flow if I have mild asthma?
If your asthma is mild and stable-with no recent flare-ups or daily medication-you can check your peak flow two to three times a week. Focus on checking when you feel different or after exposure to known triggers. But if you start having symptoms or your rescue inhaler use increases, switch to daily tracking until things stabilize.
Can I use any peak flow meter, or do I need a specific brand?
You must use the same peak flow meter every time. Different brands give different readings-even if they look identical. Switching meters will mess up your personal best and zone calculations. If you need a new one, get the same model. Bring your current meter to every doctor visit so they can compare readings directly.
What if my peak flow is normal but I’m still having trouble breathing?
If you’re wheezing, coughing, or feeling tight in your chest but your peak flow is normal, trust your symptoms. Peak flow measures large airway flow, not small airway inflammation or mucus buildup. Use your rescue inhaler as directed. If symptoms don’t improve, call your doctor. Your body is giving you important signals-don’t ignore them just because the number looks okay.
How do I know if my peak flow meter is working right?
If your readings suddenly drop by more than 10% without a change in symptoms or meds, your meter might be faulty. Try blowing into it with maximum effort-your personal best should be close to what you measured when you first set it. If you’re still unsure, bring it to your doctor. They can compare it to a clinic-grade device. Also, clean it regularly with warm water and let it dry completely-dirt or saliva can clog the mechanism.
Is peak flow monitoring useful for children with asthma?
Yes, but it requires more support. Children under 5 often can’t blow hard enough for accurate readings. For older kids, it’s very useful-especially if they don’t recognize early symptoms. Establish their personal best when they’re feeling well, and recheck it every six to twelve months as they grow. Use colorful charts or apps to make tracking fun. Always supervise their technique until they’re consistent.


Comments
Grant Hurley
Been using a peak flow meter for 3 years now and honestly? Game changer. I used to wait until I was gasping before grabbing my inhaler. Now I see the drop at 380 and I’m already on my controller. No more ER trips. No more panic. Just data. Simple as that.
On December 1, 2025 AT 11:08
Lucinda Bresnehan
My 10-year-old started using one last year after a bad attack. We made a chart with stickers - green for ‘rockstar breathing,’ yellow for ‘uh oh,’ red for ‘call mom NOW.’ She checks it every morning like it’s brushing her teeth. She even corrects me when I forget to log her evening reading. Kids are way better at consistency than adults 😅
On December 3, 2025 AT 04:03
Declan O Reilly
Y’know what’s wild? People think asthma is just wheezing. Nah. It’s the silent drop in flow that gets you. I had a buddy who swore he didn’t need tracking ‘cause he felt fine. One morning he woke up at 280, didn’t even realize it till his wife found him blue. He’s lucky to be alive. Peak flow ain’t just a tool - it’s your body’s last whisper before the scream.
On December 3, 2025 AT 14:46
Shannon Gabrielle
Oh good, another article telling us to do more work because doctors are too lazy to give us spirometry. 🙄 So now I gotta blow into a plastic tube twice a day, track it in an app, compare zones, and still pay $200 for a new meter when the old one breaks? Thanks, healthcare system. I’ll just keep breathing through it like a normal person.
On December 3, 2025 AT 22:41
patrick sui
Just a quick note on calibration - if you’re using a digital meter, make sure the firmware’s updated. I had mine drifting 15% low because of a buggy update. Took me 3 weeks to notice. Also, saliva buildup is a silent killer. Clean it daily with warm water + a toothbrush. Don’t let it get gunky. Pro tip: rinse it after each use, don’t just wipe. It’s not that hard, folks. 🤓
On December 5, 2025 AT 05:48
Dennis Jesuyon Balogun
As a pulmonology tech in Lagos, I’ve seen this save lives in places where spirometers are luxury items. One kid in Port Harcourt - 12 years old, no meds, no clinic access - used a $15 peak flow meter his uncle brought from Dublin. He tracked his zones for 8 months. When his numbers dropped below 50%, his aunt took him to the hospital. They found his airways 80% blocked. He’s alive because he had a number. Not a prayer. A number.
On December 6, 2025 AT 17:14
Matt Dean
Anyone who says peak flow is useless hasn’t had a real asthma attack. I’ve been in the hospital twice because I thought I was fine. Now I log every reading like my life depends on it - because it does. If you’re not tracking, you’re gambling. And the house always wins.
On December 7, 2025 AT 03:46
ANN JACOBS
While I appreciate the practical guidance offered in this piece, I must emphasize that the psychological dimension of chronic illness self-management cannot be understated. The act of daily measurement fosters a sense of agency, a reclamation of autonomy in the face of physiological unpredictability. Moreover, the ritualistic nature of recording one’s peak flow - whether analog or digital - serves as a form of embodied mindfulness, anchoring the individual within the temporal flow of their own physiological narrative. One must not underestimate the therapeutic value of the act itself, beyond the numerical output.
On December 8, 2025 AT 22:13
Conor Forde
Let’s be real - peak flow meters are basically glorified party tricks. I blew so hard once I nearly launched the thing across the room. My numbers were wild - 500 one day, 290 the next. Turns out I was blowing like I was trying to win a contest, not measure lung function. Then I watched a nurse do it - calm, controlled, like she was blowing out a candle on a birthday cake. Her numbers were consistent. I’ve been doing it her way since. Don’t be a hero. Be precise.
On December 10, 2025 AT 00:50
Sean McCarthy
I don't trust these things. My numbers are always weird. I think the meter is broken.
On December 10, 2025 AT 13:59