When your liver is damaged, especially from cirrhosis, blood doesn’t flow through it the way it should. That’s when portal hypertension kicks in - a silent but dangerous rise in pressure inside the main vein that carries blood from your intestines to your liver. It’s not a disease on its own. It’s a consequence. And left unchecked, it can lead to bleeding varices, fluid buildup in your belly (ascites), and even organ failure. If you or someone you care about has liver disease, understanding this condition isn’t just helpful - it’s life-saving.
What Exactly Is Portal Hypertension?
Portal hypertension means the pressure in the portal vein - the big blood vessel that brings blood from your stomach, intestines, spleen, and pancreas to your liver - has climbed above 10 mmHg. Normal pressure? Between 5 and 10 mmHg. Once it hits 10 or higher, that’s when complications start showing up. The real gold standard for measuring it? The hepatic venous pressure gradient, or HVPG. Anything above 5 mmHg is considered portal hypertension. Above 10 mmHg? That’s clinically significant. And at that point, your risk of bleeding or fluid buildup jumps dramatically.Why does this happen? In most cases - about 90% - it’s because of cirrhosis. Scar tissue builds up in the liver, squeezing the blood vessels inside. Blood can’t flow through easily, so pressure builds up behind it. The rest? Non-cirrhotic causes like blood clots in the portal vein, certain infections, or rare conditions. But cirrhosis is the big one. And if you’ve been diagnosed with cirrhosis, there’s a 70% chance you’ll develop clinically significant portal hypertension within five years.
Varices: The Hidden Time Bomb
As pressure builds in the portal system, blood looks for other ways out. It finds them - in the veins of your esophagus and stomach. These veins swell up, becoming fragile, twisted, and ready to burst. These are varices. About half of all people with cirrhosis develop them within 10 years. And when they bleed? It’s a medical emergency.Once a varix bleeds, the chance of bleeding again within a year is 60% if you don’t get proper treatment. That’s why prevention isn’t optional. The first line? Non-selective beta-blockers like propranolol or nadolol. They don’t cure the pressure, but they lower the risk of first bleeding by 45%. The goal? Reduce your resting heart rate by 25% or hit a daily dose of 160 mg of propranolol. It’s not about feeling tired - it’s about protecting your veins.
But if varices are already large, or you’ve bled before, beta-blockers alone aren’t enough. Endoscopic band ligation - where a doctor places tiny rubber bands around the swollen veins during an endoscopy - cuts rebleeding rates from 60% down to 20-30%. It’s done within 12 hours of a bleed, along with antibiotics (usually ceftriaxone) and drugs like terlipressin or octreotide to slow blood flow to the area. This combo saves lives. But it’s not perfect. You need at least 50 supervised procedures to get good at it. And even then, some varices come back.
Ascites: When Your Belly Swells for No Clear Reason
Another major complication? Ascites - fluid pooling in your abdomen. Around 60% of people with cirrhosis develop it within 10 years. At first, it might just feel like you’ve gained weight or your clothes are tighter. But as it grows, you’ll feel full fast, have trouble breathing, and get constant pain. It’s not just uncomfortable - it can lead to infection (spontaneous bacterial peritonitis) and kidney failure.Management starts simple: cut sodium. Less than 2,000 mg a day. No processed food, no canned soups, no soy sauce. Then, diuretics - spironolactone (100 mg/day) and furosemide (40 mg/day). Together, they help your kidneys flush out the extra fluid. For most people, this works. But if your belly is rock-hard and you’re struggling to breathe? You need a paracentesis - a needle inserted into your abdomen to drain the fluid. But here’s the catch: every time you remove more than 5 liters, you must get albumin (a protein) infused to prevent your blood pressure from crashing. It’s a 10- to 15-minute procedure, but it needs to be done by someone trained. Do it wrong, and you risk infection or bleeding.
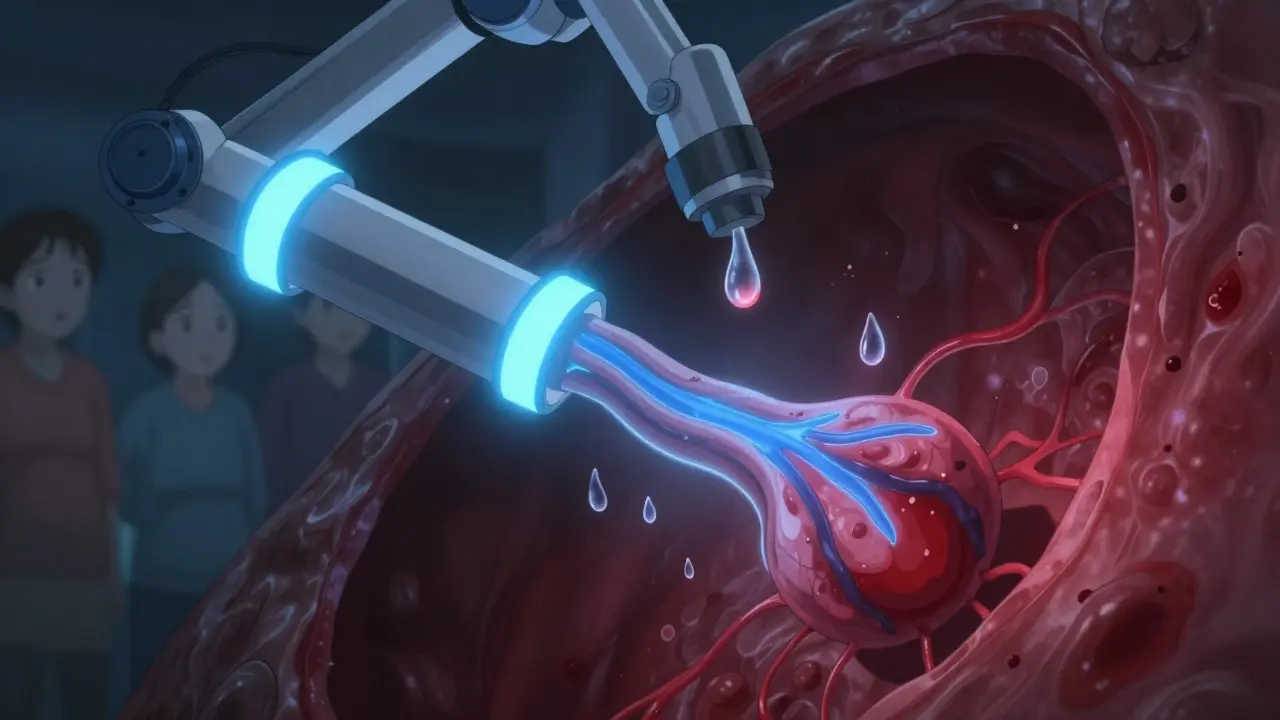
For the 10% who develop refractory ascites - fluid that won’t respond to diuretics or keeps coming back - TIPS (transjugular intrahepatic portosystemic shunt) becomes the next step. A stent is placed inside the liver to create a new channel, diverting blood away from the high-pressure portal system. It works - 90-95% of cases see major improvement. But there’s a trade-off: 20-30% of patients develop hepatic encephalopathy - confusion, memory issues, even coma - because toxins that used to be filtered by the liver now bypass it entirely.
Other Complications You Can’t Ignore
Portal hypertension doesn’t stop at varices and ascites. It sets off a chain reaction.Hepatic encephalopathy affects 30-45% of people with cirrhosis. It’s caused by toxins like ammonia building up in your blood because your liver can’t clean them out. You might feel forgetful, sluggish, or confused. Sometimes, it’s mistaken for dementia. Lactulose and rifaximin are the go-to treatments - they help your gut flush out ammonia before it reaches your brain.
Hepatorenal syndrome is even scarier. It’s when your kidneys start shutting down because of the blood flow changes caused by portal hypertension. It happens in 18% of hospitalized cirrhotic patients with ascites. There’s no fix except liver transplant. Vasoconstrictors like terlipressin and albumin can buy time, but it’s temporary.
And then there’s the emotional toll. Patients on forums talk about quitting jobs because they can’t stand for more than 20 minutes. Others live in fear of vomiting blood. Studies show their quality-of-life scores are 35-40 points lower than healthy peers. It’s not just physical - it’s psychological.
New Hope on the Horizon
The good news? Things are changing. In 2023, the FDA approved a new device called the Hepatica SmartBand - a wearable that estimates portal pressure using bioimpedance, without needing a needle in your neck. It’s 82% accurate compared to HVPG. That means fewer invasive tests.Non-invasive tools like FibroScan and spleen stiffness measurements are now hitting 85% accuracy in predicting high-risk portal hypertension. That’s huge. It could replace HVPG for many patients.
Drugs are coming too. Simtuzumab, a monoclonal antibody targeting liver scarring, showed a 35% drop in portal pressure in phase 3 trials. Twelve other drugs are in phase 2 testing, aiming to reduce pressure without dropping blood pressure too low - a major flaw in current treatments.
And AI? Mayo Clinic’s model can predict who’s most likely to bleed from varices with 92% accuracy. That means we can target high-risk patients before disaster strikes.

What You Can Do Right Now
If you have cirrhosis or chronic liver disease:- Ask for an HVPG test if you haven’t had one - it’s the only way to know your true risk.
- Get screened for varices with an endoscopy every 2-3 years (or sooner if you’re high risk).
- Take beta-blockers as prescribed - even if you feel fine.
- Stick to a low-sodium diet. No exceptions.
- Know the signs of bleeding: vomiting blood, black tarry stools, dizziness.
- Know the signs of infection from ascites: fever, abdominal pain, confusion.
Don’t wait for symptoms. Portal hypertension doesn’t warn you. It just happens. And by the time you feel it, it’s already advanced.
When Is a Liver Transplant the Only Option?
For some, no drug, no band, no shunt will fix it. When varices keep bleeding despite treatment, when ascites won’t stop coming back, when kidneys start failing - transplant becomes the only real solution. In the U.S., the average wait for a liver is 14 months. But eligibility depends on your Model for End-Stage Liver Disease (MELD) score - a calculation based on bilirubin, creatinine, and INR. Higher score? Higher priority. And portal hypertension complications raise your score fast.Transplant doesn’t cure portal hypertension - it replaces the organ causing it. After transplant, portal pressure normalizes. Varices shrink. Ascites disappears. Quality of life improves dramatically. But it’s not for everyone. You need to be healthy enough to survive surgery. And you need to commit to lifelong medications and checkups.
Can portal hypertension be cured?
No, portal hypertension itself can’t be cured - it’s a consequence of liver damage. But its complications can be managed, and in some cases, reversed. A liver transplant is the only way to eliminate the root cause. Until then, treatment focuses on lowering pressure, preventing bleeding, and controlling fluid buildup.
How do I know if I have varices?
You won’t feel them. Varices are silent until they bleed. The only way to detect them is through an upper endoscopy. If you have cirrhosis, your doctor should schedule this screening every 2-3 years. If you’ve had a bleed before, you’ll need it every year.
Are beta-blockers safe if I have asthma?
Traditional beta-blockers like propranolol can worsen asthma. But carvedilol - a non-selective beta-blocker with additional effects - is often safer and just as effective for portal hypertension. Talk to your hepatologist. There are alternatives, but don’t stop medication without medical advice.
Can I drink alcohol if I have portal hypertension?
Absolutely not. Alcohol accelerates liver scarring and increases portal pressure. Even small amounts can undo years of treatment. Abstinence is non-negotiable.
How often do I need to see a specialist?
If you’re stable, every 6 months. If you’ve had a bleed, ascites, or encephalopathy, you need to be seen every 3 months. Regular monitoring with blood tests, ultrasounds, and sometimes endoscopy is essential to catch problems before they become emergencies.
Final Thoughts
Portal hypertension is a silent storm brewing inside your body. It doesn’t shout. It doesn’t hurt - until it’s too late. But knowledge gives you power. Knowing your HVPG, watching for varices, controlling sodium, taking your meds, and staying in touch with your liver specialist can mean the difference between living with this condition - and being controlled by it.The tools are better than ever. The science is advancing. And for those who act early, the future isn’t just about survival - it’s about living well, even with a damaged liver.


Comments
Alec Amiri
So basically if you have cirrhosis, you’re just waiting for your body to betray you? Cool. I’ll just drink my beer and hope for the best. 😅
On January 21, 2026 AT 18:13
Lana Kabulova
Wait-so beta-blockers reduce bleeding risk by 45%? That’s huge-but what about the side effects? Fatigue? Dizziness? Depression? Nobody talks about how these meds make you feel like a zombie… and then you’re told to just ‘take it as prescribed’ like it’s a vitamin. Where’s the nuance?
On January 22, 2026 AT 07:15
Rob Sims
Of course the article says ‘abstain from alcohol’-like anyone with cirrhosis hasn’t already been told that 17 times. But let’s be real: the real problem is that doctors keep treating the symptoms instead of the root cause-because nobody wants to admit that most of this is just poor lifestyle choices. You made your bed. Now lie in it.
On January 23, 2026 AT 11:04
arun mehta
Thank you for this clear, compassionate breakdown 🙏
As someone from India, where liver disease is rising fast due to alcohol, diabetes, and lack of screening-I see this daily. Early detection saves lives. Please, if you’re at risk, get tested. No shame. Just action. 💪❤️
On January 23, 2026 AT 22:27
Chiraghuddin Qureshi
India has over 40 million people with chronic liver disease. We need more community screening camps, not just fancy tech. Also, many can’t afford albumin after paracentesis. 🤔
On January 24, 2026 AT 21:32
Patrick Roth
Hold on. You say ‘HVPG is the gold standard’-but it’s invasive, expensive, and only available in academic centers. Meanwhile, FibroScan is 85% accurate and costs $200. Why are we still clinging to 1980s tech? This article feels like a pharma ad.
On January 26, 2026 AT 09:12
Lauren Wall
Low sodium? No exceptions. That’s it. That’s the whole post.
On January 27, 2026 AT 09:50
Kenji Gaerlan
so like… if u got cirrhosis n u dont drink anymore, does it still count? like, did u mess up or was it just bad luck? idk man
On January 29, 2026 AT 03:51
Oren Prettyman
While the article presents a comprehensive overview of portal hypertension and its complications, it is critically deficient in addressing the socioeconomic determinants of liver disease progression. The assumption that patients have equal access to endoscopic band ligation, TIPS procedures, or even diuretics is not only naive but ethically problematic. In the United States alone, over 30% of cirrhotic patients lack consistent primary care access. Furthermore, the emphasis on patient compliance-‘take your meds’-ignores the reality of medication non-adherence driven by cost, transportation barriers, and systemic neglect. A truly evidence-based discussion must include policy-level interventions, not just clinical algorithms.
On January 29, 2026 AT 14:26
Tatiana Bandurina
You say ‘know the signs of bleeding’-but what if you’re elderly, alone, and don’t have anyone to notice you’re pale and dizzy? Or if you’re homeless and can’t afford to go to the ER? This article sounds like it was written for people who have insurance, a family, and a phone. What about the rest of us?
On January 31, 2026 AT 11:55
Philip House
They’re selling you hope with AI models and wearable bands. But let’s be honest-this is just capitalism repackaging death as innovation. The liver doesn’t care about your app. It just dies. And they’ll charge you $12,000 for a TIPS before they even mention transplant eligibility. This isn’t medicine. It’s a business model.
On February 1, 2026 AT 00:25
Ryan Riesterer
Portal pressure gradient >10 mmHg correlates with decompensation risk (HR 4.2, 95% CI 2.8–6.1). Non-selective beta-blockers reduce first bleeding by 45% (NNT 6). Band ligation reduces rebleeding to 20-30% vs. 60% without intervention. TIPS improves ascites control in >90% but carries 20-30% encephalopathy risk. HVPG remains the reference standard. FibroScan and spleen stiffness show promising AUCs >0.85. Hepatica SmartBand: 82% concordance in validation cohort. Simtuzumab phase 3: -35% HVPG reduction. Lactulose + rifaximin: 50% reduction in HE episodes. MELD >15 triggers transplant listing. These are not opinions. These are numbers.
On February 2, 2026 AT 07:01
Akriti Jain
They’re hiding the truth. The real cause? 5G towers. They interfere with liver cell signaling. That’s why it’s worse in cities. And the ‘new devices’? Just tracking you. They don’t want you to heal-they want you hooked on meds and scans forever. 🕵️♀️📱
On February 2, 2026 AT 12:57
Mike P
Bro, if you’ve got cirrhosis, you already lost. But hey, at least you can still enjoy a good steak and a cold one before the end. Live hard, die young, right? 😎
On February 4, 2026 AT 07:58
Jasmine Bryant
I just got diagnosed with cirrhosis last month. I didn’t know varices were silent until I read this. I’m getting my endoscopy next week. Thank you for the clear info. I didn’t realize how urgent this was. I’ll cut the salt. I’ll take the meds. I’ll go to my appointments. You just saved me from making a huge mistake.
On February 4, 2026 AT 10:52
Alec Amiri
Wow, Jasmine, I’m glad you’re taking this seriously. I was being a jerk earlier. You’re right-this isn’t a game. I’m getting screened too. Thanks for calling me out gently.
On February 6, 2026 AT 00:29