When Your Skin and Joints Both Betray You
Imagine waking up with stiff fingers, swollen toes, and a patch of red, scaly skin you didn’t have yesterday. You think it’s just dry skin or maybe a bad night’s sleep. But then the pain in your knee doesn’t go away. And your nail starts lifting off the bed. That’s when you realize: this isn’t just one problem. It’s two - and they’re connected.
This is psoriatic arthritis. It doesn’t just affect your joints or your skin. It attacks both at the same time. About 30% of people with plaque psoriasis - the most common skin form - will eventually develop joint pain. For some, the joints hurt first. For others, the skin flare-up comes first. But no matter the order, they’re part of the same disease.
It’s not just arthritis. It’s not just psoriasis. It’s both. And if you ignore one, the other gets worse.
How the Skin and Joints Talk to Each Other
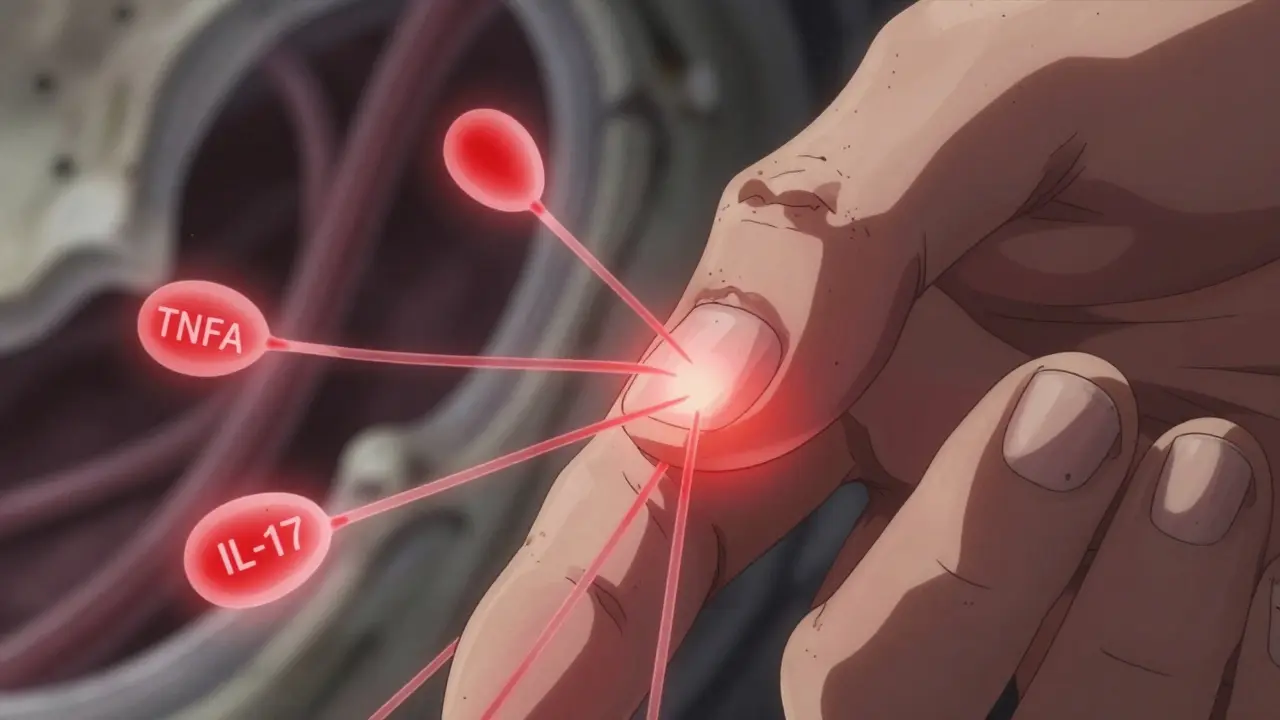
The immune system in psoriatic arthritis gets confused. It thinks healthy skin and joint tissue are invaders. So it sends inflammatory cells to attack them. That’s why you get scaly patches on your elbows and swelling in your knuckles - same root cause, different targets.
Doctors call this a systemic autoimmune disease. That means the inflammation doesn’t stay put. It travels. The same proteins that cause skin flares - like TNF-alpha and IL-17 - also attack the lining of your joints, the tendons where they connect to bone, and even your nails.
That’s why nail changes are such a big clue. If you have pitting, thickening, or your nail is pulling away from the bed (onycholysis), you’re far more likely to have joint damage. About 80-90% of people with psoriatic arthritis have nail problems. In regular psoriasis, only 10-50% do. That’s not coincidence. That’s a warning sign.
And it’s not just your hands. Your spine can get involved. Your heels. Your lower back. The inflammation doesn’t care where it shows up - as long as it can cause damage.
Signs You Can’t Ignore
Not all joint pain is the same. Rheumatoid arthritis? Usually symmetric - both wrists, both knees. Psoriatic arthritis? Often random. One knee swells. The other stays fine. One finger turns sausage-like. The rest look normal. That’s called dactylitis. It happens in 40-50% of cases. It’s unmistakable. And it’s rare in other forms of arthritis.
Another red flag: enthesitis. That’s when tendons or ligaments pull away from the bone and get inflamed. Think of it like fraying rope at the anchor point. You’ll feel pain at the back of your heel (Achilles tendon), the bottom of your foot (plantar fascia), or where your ribs meet your breastbone. It’s not just soreness. It’s sharp, deep, and gets worse when you move.
Then there’s the pattern. About 70% of people have asymmetric oligoarthritis - meaning fewer than five joints, and they’re not mirrored on both sides. Only 25% have symmetric polyarthritis, which looks more like rheumatoid arthritis. The rest fall into rarer types: spine-dominant (spondylitis), nail-focused (distal interphalangeal), or the rare but devastating arthritis mutilans, which eats away at bone.
And here’s the kicker: there’s no blood test that confirms it. No rheumatoid factor. No anti-CCP. Bloodwork often comes back normal. That’s why so many people wait years for a diagnosis. One survey found patients saw three doctors on average before getting the right name for what they had.
What Happens If You Wait
Delaying treatment isn’t just about discomfort. It’s about permanent damage.
Studies show that 30% of people with untreated psoriatic arthritis develop visible joint destruction within two years. That’s not just pain. That’s deformed fingers. That’s fused spine. That’s walking with a limp because your heel bone is eaten away.
Dr. Laura Coates at the University of Oxford found that starting treatment within 12 weeks of the first joint symptom cuts the risk of irreversible damage by 75%. That’s not a small win. That’s life-changing.
And it’s not just the joints. People with psoriatic arthritis have a 1.5 times higher risk of heart disease. The same inflammation that attacks your skin and joints also damages your arteries. Fatigue, brain fog, depression - those aren’t just side effects. They’re part of the disease.
Waiting to act isn’t patience. It’s gambling with your future mobility.
Treatment: From Pills to Injections
Treatment has changed dramatically since the 2000s. Back then, the only options were NSAIDs for pain and methotrexate - a slow, often poorly tolerated drug. Now, we have targeted therapies that stop the inflammation at its source.
DMARDs like methotrexate and sulfasalazine are still used, especially in milder cases. But they’re not enough for most people anymore.
Biologics are the game-changers. These are injectable or infused drugs that block specific parts of the immune system. TNF inhibitors like adalimumab (Humira) and etanercept (Enbrel) were the first. Now we have drugs that target IL-17 (secukinumab, ixekizumab) and IL-23 (guselkumab, risankizumab). These work faster and often clear skin better than older drugs.
And in 2022, the FDA approved deucravacitinib (Sotyktu), the first oral TYK2 inhibitor for psoriatic arthritis. No needles. Just a daily pill. Early results show 58% of patients hit a 20% improvement in symptoms at 16 weeks.
But here’s the catch: not all drugs work for everyone. One patient on Reddit said ustekinumab (Stelara) wiped out his joint pain - but gave him a scalp flare. Another switched to guselkumab (Tremfya) and went from two hours of morning stiffness to 20 minutes.
That’s why treatment is personalized. It’s trial and error - but now it’s faster. Doctors use tools like the PsAID (Psoriatic Arthritis Impact of Disease) score to track progress. The goal? Minimal disease activity. Not just less pain. Less swelling. Less fatigue. Less skin.

Who Treats This - And How
You need more than one specialist. A rheumatologist handles the joints. A dermatologist handles the skin. But the best outcomes come when they work together.
Studies show 85% of effective treatment plans involve both. That’s because skin flares often predict joint flares. If your dermatologist sees a new patch of psoriasis, they should alert your rheumatologist. If your rheumatologist sees new joint swelling, they should check your nails and scalp.
Physical therapists are part of the team too. They teach you exercises to keep joints mobile without causing more damage. Occupational therapists help with daily tasks when your hands are stiff.
And don’t underestimate lifestyle. Weight loss cuts inflammation. Smoking makes it worse. Alcohol interferes with medications. Exercise - even walking - improves joint function and reduces fatigue.
Cost, Access, and the Hidden Struggles
These drugs work. But they’re expensive. Biologics can cost over $500 a month out-of-pocket. Insurance approvals take an average of 14.7 business days. Many patients delay treatment because they can’t afford it - or their insurer won’t approve it.
Injection site reactions happen in 65% of people using subcutaneous biologics. That’s redness, itching, burning. Not life-threatening, but enough to make some people skip doses.
And then there’s brain fog. Fifty-two percent of patients report it persists even when their joints feel better. It’s not just tiredness. It’s trouble focusing, memory lapses, mental sluggishness. Doctors are starting to take it seriously. It’s linked to inflammation in the brain, not depression.
There’s hope. New oral drugs are coming. AI tools can now predict who’ll develop psoriatic arthritis from psoriasis with 87% accuracy using nail images and joint scans. By 2028, genetic testing may tell you which drug will work best for you - cutting out the trial-and-error phase.
What You Can Do Today
If you have psoriasis and notice joint pain, swelling, or stiffness - don’t wait. Don’t assume it’s aging. Don’t think it’s just overuse.
Track your symptoms. Write down when your joints hurt, which ones, how long it lasts, and if your skin changes at the same time. Take photos of new rashes or nail changes. Bring this to your doctor.
Ask: Could this be psoriatic arthritis? If your doctor says no, ask for a referral to a rheumatologist. You have the right to a second opinion.
Start with your skin. If your dermatologist hasn’t checked your joints, ask them to. If your rheumatologist hasn’t looked at your nails, ask them to. This disease doesn’t live in one place. Your care shouldn’t either.
You don’t have to live with pain that gets worse. You don’t have to wait years for answers. The tools to stop this disease exist. You just need to speak up - and get the right team behind you.

