Proctitis Symptom Impact Calculator
How Smoking Affects Your Proctitis Symptoms
Enter your current smoking habits and see the estimated impact on your proctitis symptoms and flare-ups.
Key Takeaways
- Smoking directly aggravates proctitis by increasing inflammation and disrupting the gut lining.
- Nicotine and other chemicals impair the immune response and alter the gut microbiome, leading to more frequent flare‑ups.
- Smokers often experience longer flare‑up duration, higher pain scores, and slower healing after treatment.
- Quitting or reducing smoking can markedly improve symptom control and reduce the need for aggressive medication.
- Targeted lifestyle changes - diet, stress management, and regular monitoring - complement smoking cessation for better outcomes.
What is Proctitis?
When we talk about Proctitis is a inflammatory condition affecting the lining of the rectum, the main symptoms are urgency, tenesmus (feeling of incomplete evacuation), bleeding, and abdominal cramping. It can appear on its own (idiopathic) or as part of a broader inflammatory bowel disease (IBD) like ulcerative colitis.
Typical triggers include infections, radiation therapy, and certain medications, but lifestyle factors - especially smoking - play a surprisingly strong role in how the disease behaves.
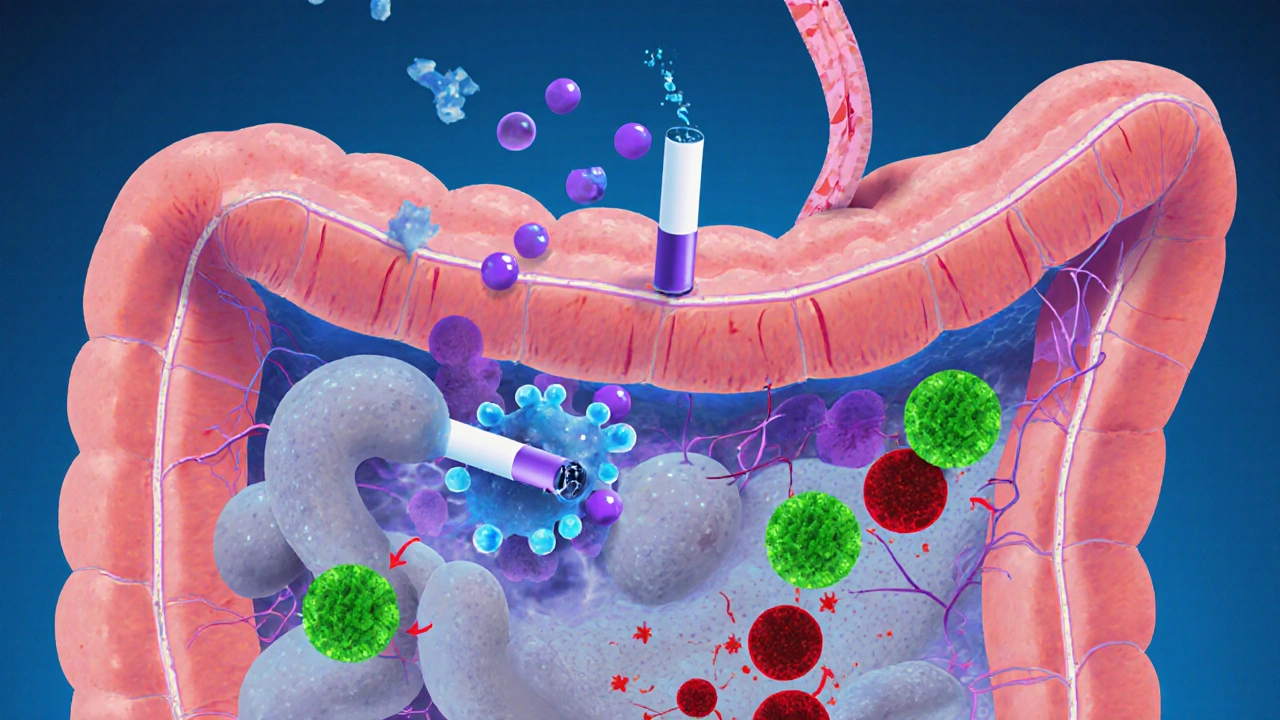
How Smoking Affects the Gut
Smoking is a complex exposure that delivers nicotine, carbon monoxide, and over 4,000 chemicals to every organ, including the gastrointestinal tract.
Two mechanisms matter most for proctitis:
- Immune modulation: Nicotine binds to receptors on immune cells, skewing them toward a pro‑inflammatory state. This is captured in the relationship Nicotine→Immune response→Increased inflammation.
- Microbiome disruption: Studies from 2023‑2024 show smokers have a lower diversity of beneficial bacteria such as Lactobacillus and a higher prevalence of pathogenic strains. The altered Gut microbiome weakens the gut barrier, making the rectal lining more vulnerable.
Both pathways create a fertile ground for flare‑ups in anyone with an already inflamed rectum.
Direct Impact of Smoking on Proctitis Symptoms
Research summarized in a 2024 meta‑analysis of 12 cohort studies found that smokers with proctitis reported:
- 28% higher pain scores during flare‑ups.
- Nearly double the risk of bleeding episodes.
- Average flare‑up duration extended by 4‑6days compared with non‑smokers.
Why does this happen? The chemicals in cigarette smoke increase vascular permeability in the rectal mucosa, leading to more bleeding. At the same time, nicotine stimulates the release of cytokines (IL‑6, TNF‑α) that keep the inflammation alive longer.
Furthermore, smokers often have reduced response to standard therapies such as Mesalamine. The drug’s ability to coat the colon wall is compromised when the mucosal surface is constantly irritated by smoke‑related toxins.
Managing Flare‑ups When You Smoke
If quitting right now feels impossible, here are practical steps to limit damage during a flare‑up:
- Hydration: Aim for at least 2liters of water daily. Proper hydration helps thin stool and reduces rectal trauma.
- Dietary fiber: Soluble fiber from oats or psyllium can form a protective gel that eases passage and shields the inflamed lining.
- Targeted medication: Discuss with your gastroenterologist the possibility of adding a short course of oral steroids or a rectal suppository containing corticosteroids during heavy smoking periods.
- Scheduled colonoscopy checks: Regular Colonoscopy monitoring helps catch worsening inflammation early, before it spirals.
- Avoid triggers: Alcohol, spicy foods, and NSAIDs can amplify smoke‑induced irritation. Keep a symptom diary to see what combos hit you hardest.
These tactics won’t eliminate the smoke’s effect, but they can shrink flare‑up intensity and shorten recovery time.
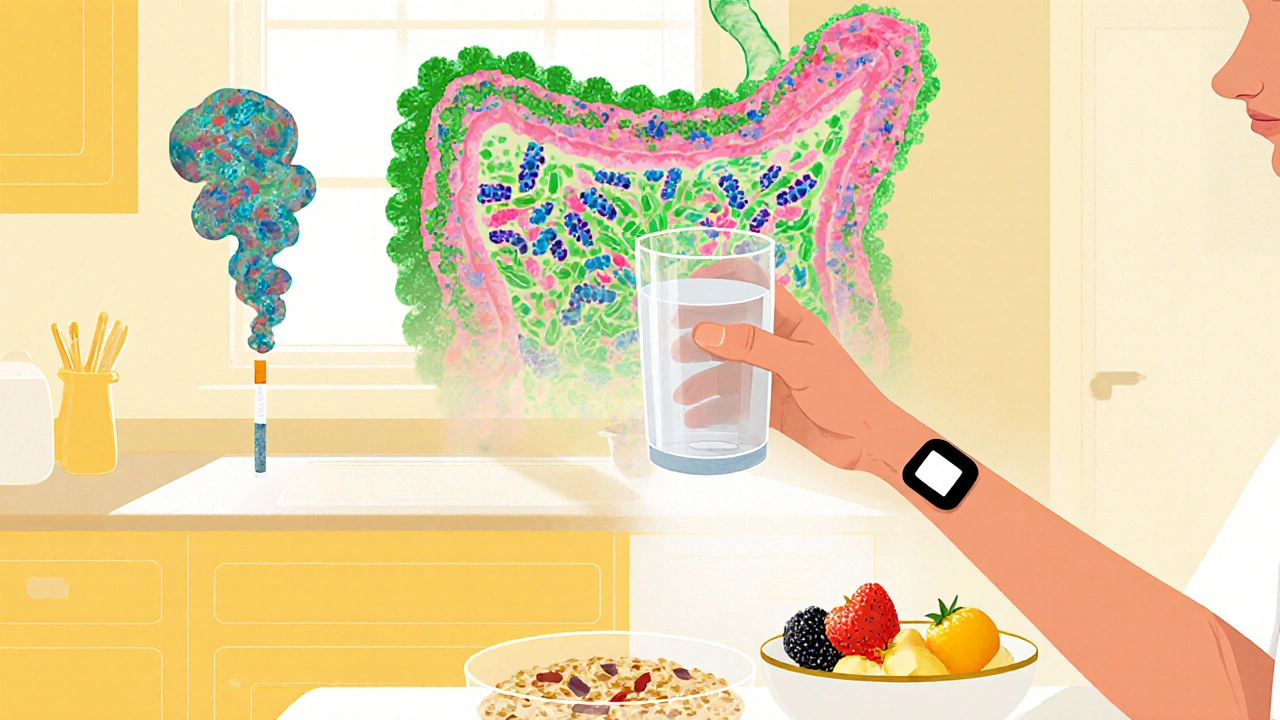
Steps Toward Smoking Reduction or Cessation
Evidence shows that even cutting down to fewer than 5 cigarettes a day can provide measurable benefits for proctitis patients. Here’s a structured plan:
- Set a realistic goal: Choose a quit date within the next 30days. Mark it on a calendar and treat it like a medical appointment.
- Replace the habit: Use nicotine‑replacement therapy (patches, gum) to blunt cravings while you focus on diet and stress reduction.
- Track progress: A simple spreadsheet listing daily cigarette count, pain score, and stool consistency reveals patterns that motivate change.
- Seek professional help: Referral to a smoking‑cessation clinic or a counselor can raise success rates from 10% to over 30%.
- Leverage community: Online forums for IBD patients often share success stories. Seeing peers who’ve quit and felt symptom relief is a powerful incentive.
Remember, quitting smoking isn’t just a lung‑health decision; it’s a gut‑health decision that directly eases proctitis.
Comparison: Smoker vs. Non‑Smoker with Proctitis
| Factor | Smoker | Non‑Smoker |
|---|---|---|
| Pain level (0‑10) | 6‑8 during flares | 3‑5 during flares |
| Average flare‑up duration | 10‑14days | 5‑8days |
| Bleeding episodes | Frequent (≥3/month) | Rare (≤1/month) |
| Response to Mesalamine | Partial (≤50% symptom relief) | Strong (≥70% symptom relief) |
| Microbiome diversity index | Low (↓20% vs. healthy) | Moderate (↓5% vs. healthy) |
These numbers illustrate why many gastroenterologists push smoking cessation as the first line of defence against worsening proctitis.
Frequently Asked Questions
Can occasional smoking still trigger a proctitis flare‑up?
Yes. Even a single cigarette can increase rectal blood flow and release irritant chemicals, which may be enough to spark a flare in a sensitised gut. The risk rises with frequency, but occasional use isn’t safe.
Is e‑cigarette use any better for proctitis?
Current evidence suggests vaping still delivers nicotine and propylene glycol, both of which can disrupt the microbiome and inflammation pathways. While it may reduce some toxicants, it does not eliminate the pro‑inflammatory effect on the rectum.
Do nicotine patches help reduce proctitis symptoms?
Nicotine patches provide a steady low dose of nicotine, which can still engage immune receptors. Some patients report milder symptoms than with cigarettes, but the best outcome is achieved when nicotine itself is eliminated.
How often should I get a colonoscopy if I smoke and have proctitis?
Guidelines recommend a surveillance colonoscopy every 1‑2years for active proctitis, but smokers may need yearly checks because the disease can progress faster. Discuss a personalized schedule with your gastroenterologist.
Can diet alone offset the damage from smoking?
A gut‑friendly diet (high soluble fiber, low processed foods) can reduce irritation, but it cannot fully counteract the systemic inflammation caused by smoking. Combining diet with smoking reduction yields the greatest benefit.


Comments
Mike Rylance
Quitting smoking can dramatically reduce proctitis flare‑ups; consider setting a concrete cessation date within the next month and treating it as a non‑negotiable medical appointment. Tracking each cigarette avoided alongside your daily pain score will make the progress visible and reinforce the habit change. Hydration and soluble fiber should accompany the quit attempt to further protect the rectal lining. Remember that nicotine replacement therapy is a bridge, not a destination, and the ultimate goal remains a smoke‑free life. Stay motivated, the benefits to your gut health are worth the effort.
On October 14, 2025 AT 12:29
Becky B
They don’t want you to know how the tobacco lobby suppresses data linking nicotine to gut inflammation; the real cure is hidden in plain sight, buried under layers of regulatory spin. Every time a cigarette is lit, chemicals flood the rectal microvasculature, worsening bleeding risk while the establishment claims it’s a personal choice. The truth is that corporate interests profit from the very flare‑ups they pretend are unrelated. By staying informed and demanding transparent research, patients can reclaim control over their own health.
On October 21, 2025 AT 11:09
Aman Vaid
Recent studies quantify nicotine’s effect on immune modulation: nicotine binds α7‑nAChR receptors, skewing macrophage polarization toward a pro‑inflammatory M1 phenotype. Concurrently, metagenomic analyses reveal a 22 % reduction in Lactobacillus spp. diversity among smokers with proctitis, compromising mucosal barrier integrity. The combined impact translates to higher IL‑6 and TNF‑α serum levels, which correlate with extended flare duration. Clinicians therefore advise cessation as an adjunct to pharmacologic therapy to restore immunologic balance.
On October 28, 2025 AT 08:49
xie teresa
I understand how frustrating these symptoms can be; many patients have found real relief after simply cutting back on cigarettes. Even a modest reduction-down to fewer than five per day-often translates into lower pain scores and shorter flare‑ups. Pairing that reduction with a high‑soluble‑fiber diet and plenty of water creates a protective barrier for the rectal lining. Keep a symptom diary; seeing the numbers improve can be a powerful motivator.
On November 4, 2025 AT 07:29
Srinivasa Kadiyala
It’s not just about nicotine, it’s about the thousands of chemicals, the tar, the carbon monoxide, each of which independently contributes to mucosal irritation, to vascular permeability, to dysbiosis, to heightened cytokine release, to delayed healing, to increased bleeding risk, to reduced response to Mesalamine, to overall disease burden, to quality‑of‑life deterioration, to a vicious cycle that is difficult to break without comprehensive cessation strategies.
On November 11, 2025 AT 06:09
Alex LaMere
Smoking adds a measurable increase in flare frequency, cessation improves response to Mesalamine. 😊
On November 18, 2025 AT 04:49
Dominic Ferraro
Think of quitting as a heroic quest for your gut: each day without a cigarette is a small victory that adds up to a massive triumph over inflammation. Start with a solid plan-pick a quit date, gather nicotine‑replacement tools, enlist a buddy for accountability. Celebrate milestones, even the tiny ones, because they signal real healing happening beneath the surface. Remember, the gut’s microbiome is resilient; give it the nourishment and calm it deserves and it will reward you with fewer flare‑ups and smoother days.
On November 25, 2025 AT 03:29
Jessica Homet
If you keep lighting up, expect more pain.
On December 2, 2025 AT 02:09
KayLee Voir
Supporting each other through these challenges makes a big difference; sharing success stories about cutting back can inspire others who feel stuck. I’ve seen friends who reduced their smoking to just social occasions and notice a noticeable dip in pain levels. Pair those changes with gentle exercise like walking, which improves circulation to the rectal tissue. Small, consistent steps often lead to the biggest health gains.
On December 9, 2025 AT 00:49
Bailey Granstrom
Stop the smoke, watch the pain melt away!
On December 15, 2025 AT 23:29
Melissa Corley
i think most people dont even realiez how bad smkng is for ur gut lol, just keep on ignitin ur habit and watch the flares keep comin 🤷♀️
On December 22, 2025 AT 22:09
Kayla Rayburn
Just a chill reminder: we all have different thresholds, so pay attention to what your body’s telling you. If a cigarette seems to make the next day feel rough, that’s a signal. No need to be hard on yourself; take it step by step.
On December 29, 2025 AT 20:49
Jack Marsh
While the data suggest a correlation between smoking and increased proctitis activity, alternative interpretations exist that emphasize the role of concurrent stressors and dietary patterns. It is therefore insufficient to attribute causality solely to nicotine exposure without controlling for these variables.
On January 5, 2026 AT 19:29
Terry Lim
The evidence is clear: if you continue to smoke, you are choosing more pain and longer flares. This is not a personal preference, it is a medical decision.
On January 12, 2026 AT 18:09
Cayla Orahood
Behind the curtain of mainstream medicine lies a hidden agenda, pushing nicotine products while downplaying their gut‑destructive power. The elite orchestrate the narrative, ensuring the public remains distracted by surface‑level advice. Only when we pull back the veil can we see that true healing requires complete detachment from the tobacco empire.
On January 19, 2026 AT 16:49
McKenna Baldock
One might contemplate the paradox of a habit that simultaneously comforts the mind yet corrodes the body’s most intimate pathways. By reflecting on the fleeting nature of nicotine’s pleasure against the enduring benefit of gut health, we arrive at a deeper understanding of self‑care as an ethical pursuit.
On January 26, 2026 AT 15:29
Roger Wing
Smoking introduces a cascade of harmful substances that collectively exacerbate proctitis, yet the prevailing discourse often reduces the conversation to a simplistic "smoke‑bad, quit‑good" mantra. First, the nicotine component interacts with α7‑nicotinic acetylcholine receptors on immune cells, biasing them toward a pro‑inflammatory M1 phenotype, which amplifies cytokine release, notably IL‑6 and TNF‑α. Second, the tar and particulate matter compromise the intestinal mucosal barrier, increasing permeability and allowing bacterial translocation that further fuels inflammation. Third, the oxidative stress generated by carbon monoxide and free radicals depletes local antioxidant defenses, reducing tissue repair capacity. Fourth, the alteration of the gut microbiome, characterized by a decline in beneficial Lactobacillus and Bifidobacterium species, creates dysbiosis that impairs short‑chain fatty acid production, essential for colonocyte health. Together, these mechanisms manifest clinically as heightened pain scores, prolonged flare‑up duration, and increased bleeding risk. While nicotine replacement therapies mitigate withdrawal, they still provide a low‑level nicotine stimulus that can sustain some degree of immune activation; complete cessation remains the most effective strategy for restoring mucosal integrity. Moreover, lifestyle interventions-adequate hydration, soluble fiber intake, and stress reduction-serve as adjuncts that can help re‑establish a resilient microbiota and improve the response to standard pharmacologic agents such as mesalamine. Ultimately, the decision to quit smoking is not merely a personal habit change but a crucial component of comprehensive proctitis management.
On February 2, 2026 AT 14:09