When you take diuretics and lithium, a combination that can dangerously raise lithium levels in your blood. Also known as lithium-diuretic interaction, this pairing is one of the most common and dangerous drug interactions in mental health and kidney care. Lithium is used to treat bipolar disorder, but it has a very narrow safety window—too little doesn’t work, too much can be life-threatening. Diuretics, often prescribed for high blood pressure or swelling, mess with how your kidneys clear lithium. That’s not a small risk. It’s a red flag.
The biggest problem comes from thiazide diuretics, a class of water pills like hydrochlorothiazide and chlorthalidone. These drugs reduce sodium in your body, which tricks your kidneys into holding onto more lithium instead of flushing it out. Studies show lithium blood levels can jump 25% to 50% within days of starting a thiazide. Even loop diuretics like furosemide can cause trouble, though less often. The result? Tremors, confusion, nausea, dizziness, or worse—seizures, kidney damage, or coma. You don’t need to stop lithium. But you do need to know what’s happening inside your body.
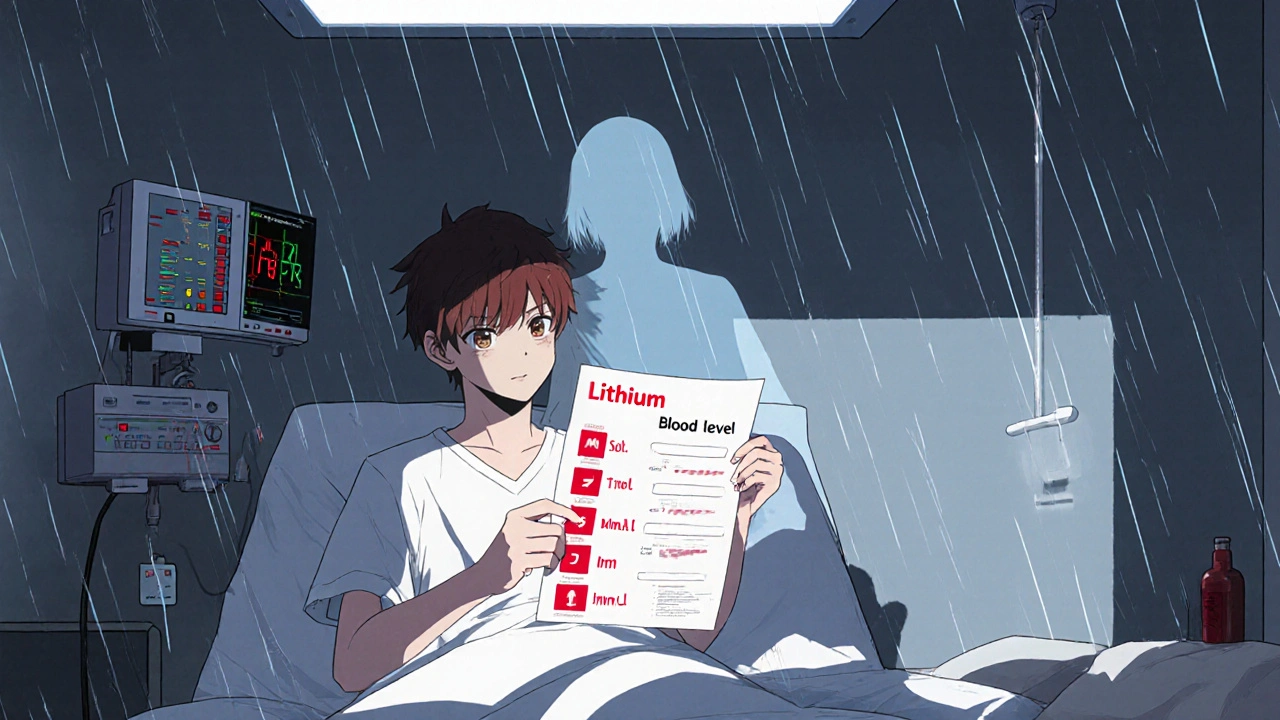
People on long-term lithium therapy are especially vulnerable. If you’ve been stable for years, adding a diuretic for high blood pressure might seem harmless. But your kidneys don’t forget how they handle lithium. And if you’re older, dehydrated, or have kidney issues, the risk goes up fast. That’s why doctors check lithium levels before and after starting a diuretic—and often every few weeks after. Blood tests aren’t optional here. They’re essential. Even over-the-counter pain meds like ibuprofen or naproxen can make things worse by cutting kidney blood flow. It’s not just one drug. It’s the whole mix.
There’s no magic fix. Some patients switch to non-diuretic blood pressure meds like ACE inhibitors or calcium channel blockers. Others stay on lithium but get daily fluid and salt monitoring. If you’re on both, never skip your lab work. Never cut back on water thinking it’ll help with swelling. Dehydration makes lithium toxicity far more likely. And if you feel off—more tired than usual, shaky, nauseous—don’t wait. Get tested. Lithium toxicity doesn’t wait.
Below, you’ll find real-world guides on how this interaction plays out in practice. You’ll see how doctors adjust doses, what alternatives exist, and how patients manage their care without risking their health. These aren’t theory pieces. They’re tools made by people who’ve been there. Whether you’re on lithium, prescribing it, or caring for someone who is, the information here could change everything.
Lithium toxicity can happen quietly when common drugs like diuretics and NSAIDs interfere with kidney function. Learn how these interactions work, which medications are most dangerous, and what steps you must take to stay safe.
Read More© 2026. All rights reserved.