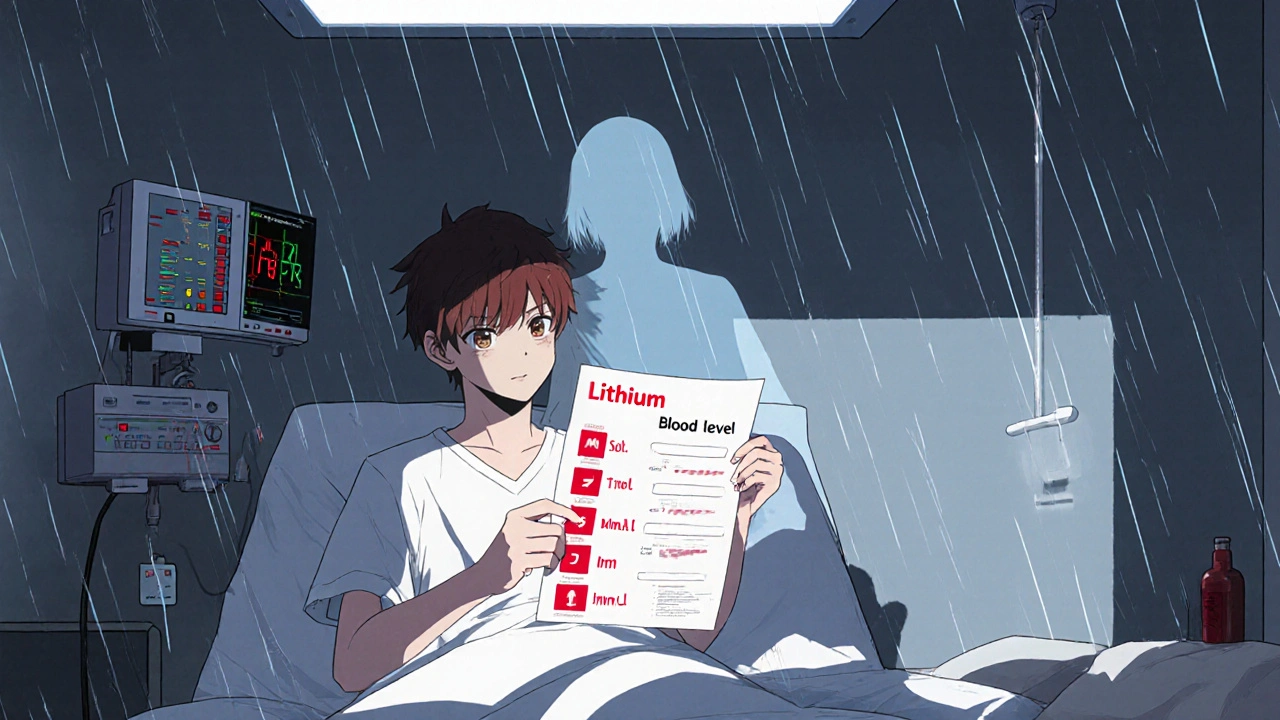
When you take lithium, a mood-stabilizing medication used primarily for bipolar disorder. Also known as lithium carbonate, it helps prevent manic and depressive episodes—but only if your blood levels stay in the narrow safe range. Too little and it won’t work. Too much and it can poison you. That’s why lithium monitoring, the regular testing of lithium levels in your blood isn’t optional—it’s life-saving.
Doctors don’t just check lithium levels once and call it done. They track them over time because your body changes. Kidney function, hydration, salt intake, even the season can shift how your body handles lithium. That’s why lithium blood levels, typically measured in millimoles per liter (mmol/L) are checked every few weeks at first, then every 3 to 6 months once stable. The sweet spot? Between 0.6 and 1.2 mmol/L. Above 1.5? That’s a red flag. Above 2.0? That’s an emergency.
And it’s not just about the number. lithium side effects, like tremors, frequent urination, or nausea are early warning signs. If you feel off, your doctor needs to test your levels—even if you’re not due for one. lithium toxicity, a dangerous buildup of the drug in your system can cause confusion, seizures, or even heart problems. It’s rare if you’re monitored, but it happens when people skip tests or change their diet or meds without telling their doctor.
That’s why tracking isn’t just about the lab report. It’s about your daily habits. Drinking less water? Eating less salt? Starting a new diuretic? These all raise your lithium levels. Your doctor needs to know. You need to know too. This isn’t a one-time conversation. It’s an ongoing partnership between you and your care team.
Below, you’ll find real-world guides on how lithium interacts with other meds, what to do when side effects show up, how kidney health affects your treatment, and what to watch for when switching therapies. No fluff. Just what works—and what could hurt you if you ignore it.
Lithium toxicity can happen quietly when common drugs like diuretics and NSAIDs interfere with kidney function. Learn how these interactions work, which medications are most dangerous, and what steps you must take to stay safe.
Read More© 2026. All rights reserved.