When you take NSAIDs, nonsteroidal anti-inflammatory drugs used for pain, swelling, and fever. Also known as non-opioid painkillers, they include common meds like ibuprofen, naproxen, and celecoxib. and you’re also on lithium, a mood-stabilizing drug used primarily for bipolar disorder. you’re playing with fire—literally. These two don’t mix well, and the danger isn’t theoretical. It’s documented, predictable, and often avoidable—if you know what to look for.
Here’s the simple truth: NSAIDs reduce blood flow to your kidneys. Lithium is cleared from your body almost entirely by your kidneys. When NSAIDs slow down kidney function, lithium doesn’t get flushed out like it should. That means lithium builds up in your blood. Levels that were safe yesterday can turn toxic today. Symptoms? Tremors, confusion, nausea, dizziness, even seizures. It’s not a side effect—it’s a medical emergency. Studies show NSAID use can raise lithium levels by 25% to 50%, sometimes more. And many people don’t realize it’s happening until they feel awful.
This isn’t just about popping an Advil for a headache. It’s about every time you reach for a pain reliever. Even a single dose of ibuprofen can trigger the problem in someone on long-term lithium. The same goes for naproxen, diclofenac, or even topical NSAIDs if you’re using them heavily. Your doctor might not warn you unless you ask. And if you’re on lithium, you need to treat every new medication like a potential landmine.
Some people think switching to acetaminophen (Tylenol) is safe. It usually is—but not always. If your kidneys are already struggling from age, diabetes, or dehydration, even acetaminophen can add stress. The real solution? Don’t guess. Talk to your prescriber before taking anything new. Keep a list of every pill, supplement, or OTC med you use. Ask: "Will this affect my lithium?" That one question could save your life.
And it’s not just about the drugs themselves. Your body’s condition matters too. Dehydration? That’s a red flag. Sweating hard during a workout? Skipping water for hours? A hot day? All of these make your kidneys work harder—and lithium harder to clear. If you’re on lithium, you need to drink water like it’s your job. Not "sometimes," not "when you’re thirsty." Daily, consistent hydration isn’t optional—it’s part of your treatment plan.
There’s also a hidden layer: many people take NSAIDs for arthritis or back pain while on lithium for mood stability. Both conditions are common. But doctors don’t always connect the dots. If your mood suddenly worsens, or you feel foggy, dizzy, or nauseous, don’t assume it’s your bipolar disorder flaring. It could be your painkiller.
What you’ll find in the posts below are real, practical guides on how these drugs behave in the body, how to spot trouble early, and what alternatives exist when you need pain relief without risking lithium toxicity. You’ll see how kidney function, hydration, and drug timing all play into this. You’ll learn what other patients have done when they had to stop NSAIDs—and what worked instead. This isn’t theory. It’s what happens when real people manage complex meds every day.
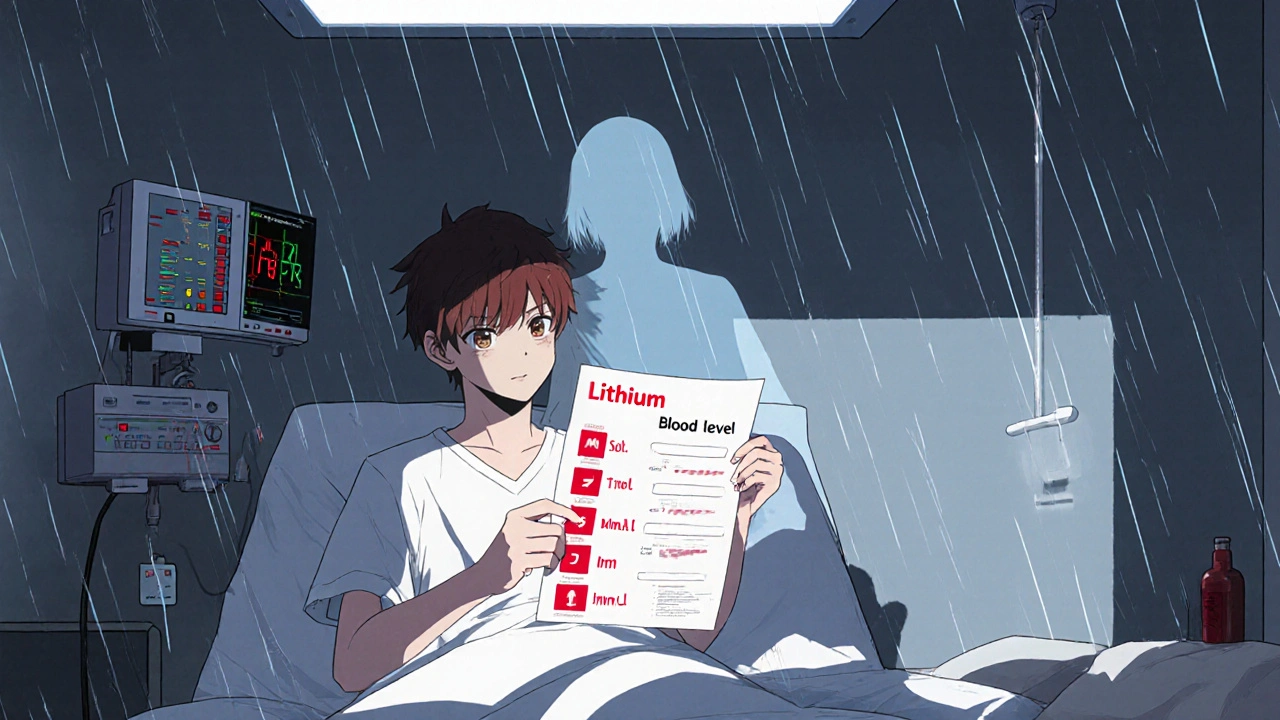
Lithium toxicity can happen quietly when common drugs like diuretics and NSAIDs interfere with kidney function. Learn how these interactions work, which medications are most dangerous, and what steps you must take to stay safe.
Read More© 2026. All rights reserved.