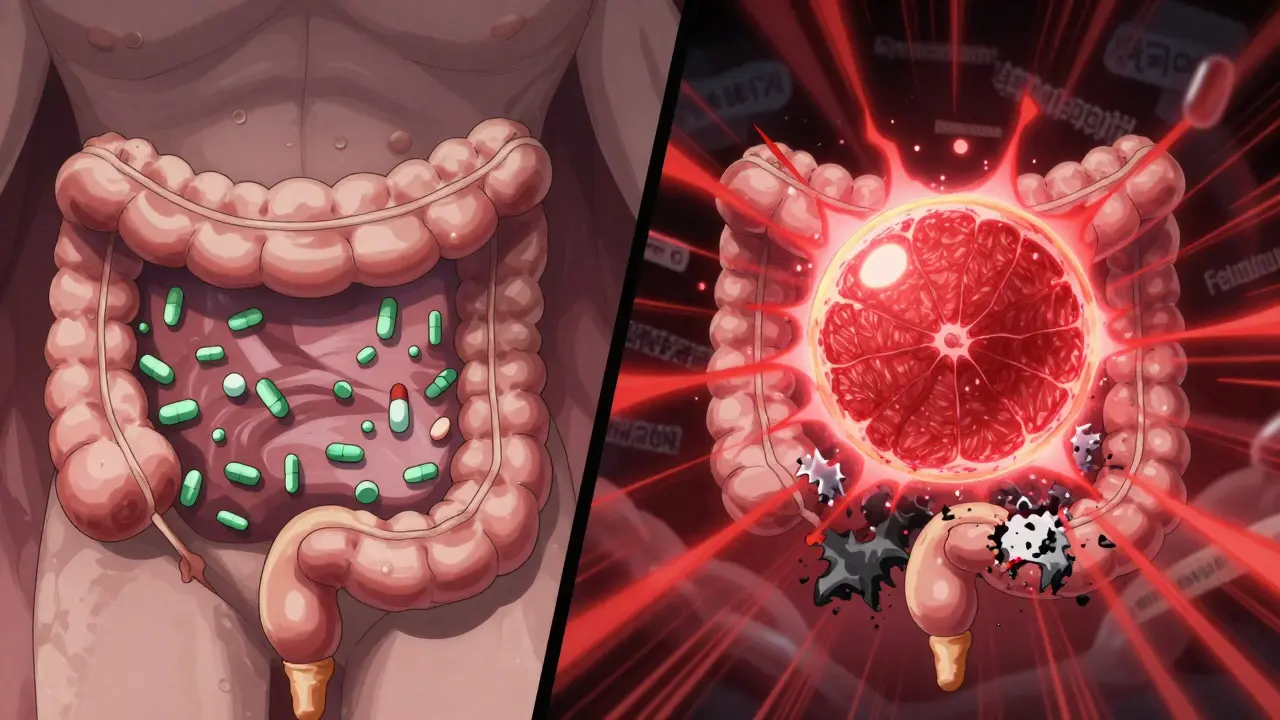
Drinking a glass of grapefruit juice in the morning might seem like a healthy habit-until it puts you in the hospital. For people taking certain medications, this citrus drink isn’t just a harmless breakfast companion. It’s a silent danger that can turn a safe dose into a toxic one. The problem isn’t about sugar or acidity. It’s about what’s hidden in the juice: chemicals that sabotage how your body processes drugs. And once this interaction happens, there’s no quick fix.
How Grapefruit Juice Changes How Your Body Handles Medicine
Back in 1989, researchers in Canada noticed something strange. Patients taking the blood pressure drug felodipine had much higher levels of the drug in their blood than expected-just because they’d had grapefruit juice with their pill. That wasn’t a coincidence. It turned out grapefruit juice blocks an enzyme in the gut called CYP3A4. This enzyme normally breaks down about half of all oral medications before they enter your bloodstream. When it’s turned off, your body absorbs way more of the drug than intended.
This isn’t a temporary glitch. The inhibition is permanent for the cells lining your intestine. Once those enzyme cells are damaged, they stay out of commission until your body makes new ones-which takes 24 to 72 hours. That means even if you take your medication at night and drink grapefruit juice in the morning, you’re still at risk. One 200-milliliter glass (about 6.7 ounces) can reduce CYP3A4 activity by nearly half within four hours. And the effect lingers long after the juice is gone.
Which Medications Are Most at Risk?
More than 85 prescription drugs are known to interact with grapefruit juice. Not all are equally dangerous, but some can be deadly. The biggest red flags are medications used for:
- High cholesterol-especially simvastatin (Zocor). A daily glass of grapefruit juice can triple the drug’s concentration in your blood. That raises your risk of rhabdomyolysis, a condition where muscle tissue breaks down and can lead to kidney failure. Studies show the risk jumps from 0.04 to 0.44 cases per 100 person-years. Atorvastatin (Lipitor) is less affected, while pravastatin and rosuvastatin show no interaction at all.
- High blood pressure-felodipine and nifedipine can see their levels spike by 5-fold and 3.3-fold respectively. Amlodipine, however, is mostly safe. The difference? It’s absorbed differently and doesn’t rely as heavily on CYP3A4.
- Heart rhythm problems-amiodarone (Cordarone) levels can rise by 30-40%, increasing the chance of dangerous arrhythmias.
- Organ transplants-cyclosporine (Neoral) levels can climb by 50-60%, raising the risk of kidney damage.
- Anxiety and sleep-some benzodiazepines and sedatives like midazolam are affected, but others like trazodone and zolpidem aren’t. Don’t assume all sleep aids are safe.
Here’s the catch: not every brand or version of a drug behaves the same. Generic versions might have different inactive ingredients that change how they’re absorbed. That’s why you can’t just assume “if one statin is okay, so are the others.”
Not All Citrus Is the Same
If you love citrus but need to avoid grapefruit, you’re not out of luck. Seville oranges (the kind used in marmalade) and pomelos contain the same furanocoumarins as grapefruit and should be avoided too. But sweet oranges-like navel or Valencia-and lemons? They’re safe. They don’t have the chemicals that block CYP3A4. Limes? Most common limes (Persian) are low risk, but bitter limes (like Key limes) may still contain enough to cause trouble.
Even processed grapefruit products aren’t safe. Pasteurized juice, frozen concentrate, or even grapefruit-flavored sodas can still contain enough furanocoumarins to trigger an interaction. The only exception? Some experimental CRISPR-edited grapefruits with 90% less of these compounds are in early testing-but they’re not on shelves yet.
Why Some People Are More at Risk
Not everyone reacts the same way. A 2013 study showed that when people drank the same amount of grapefruit juice with felodipine, drug levels ranged from zero to eight times higher than normal. Why? Because people naturally have different levels of CYP3A4 in their intestines. Those with higher baseline levels get hit harder. Age matters too-people over 65 are more likely to be on multiple medications and consume grapefruit regularly. In fact, older adults make up 40% of grapefruit juice drinkers in the U.S., according to USDA data.
There’s no test to measure your personal CYP3A4 activity. So doctors can’t tell you in advance if you’re in the 10% who’ll have a mild reaction or the 5% who’ll have a life-threatening one. That’s why the safest rule is universal: if your drug is on the list, avoid grapefruit entirely.
What About Over-the-Counter Drugs and Supplements?
You might think only prescription meds are dangerous. But some OTC drugs and supplements can also interact. Fexofenadine (Allegra), an antihistamine, is less absorbed when taken with grapefruit juice-meaning it might not work as well. Melatonin, certain herbal supplements like St. John’s wort, and even some cough syrups can be affected too. And here’s the kicker: many people don’t realize their supplements are drugs. The FDA doesn’t require supplement labels to list interactions the way prescription drugs do.
That’s why it’s critical to tell your pharmacist every pill, capsule, or tea you take-even if you think it’s “natural” or “harmless.” A 2021 study found that 89% of community pharmacists actively screen for grapefruit interactions when dispensing meds. But only 38% of patients remember being warned.

What Should You Do?
If you’re on any medication, here’s your action plan:
- Check your label. Look for the grapefruit warning. By 2023, 76% of affected drug labels include a clear “avoid grapefruit” notice. If it’s not there, don’t assume it’s safe.
- Ask your pharmacist. They have access to updated interaction databases and can flag risks you might miss.
- Keep a full list of everything you take. Include prescriptions, OTC drugs, vitamins, and herbal products. Bring it to every appointment.
- Ask about alternatives. If you love grapefruit and take simvastatin, ask if switching to pravastatin or rosuvastatin is an option. For blood pressure, amlodipine is often a safer choice than felodipine. For transplant patients, tacrolimus may be preferred over cyclosporine.
- Don’t wait for symptoms. You won’t feel the interaction happening. Muscle pain, confusion, irregular heartbeat, or sudden fatigue could be early signs of toxicity.
Why This Isn’t Just a “Be Careful” Warning
Dr. David Bailey, who discovered this interaction in 1989, put it plainly: “For susceptible drugs, a single glass of grapefruit juice can be the difference between therapeutic benefit and a fatal arrhythmia.” This isn’t hypothetical. There are documented cases of people dying from heart rhythm problems after drinking grapefruit juice with their heart meds.
The FDA, Mayo Clinic, Harvard Medical School, and the European Medicines Agency all agree: the risk isn’t worth it. You can’t predict who will react badly. You can’t time it around your dose. And you can’t rely on “just a little.” Even a small amount can trigger a reaction that lasts days.
That’s why the official advice isn’t “avoid grapefruit around the time you take your pill.” It’s “avoid grapefruit the whole time you’re on the medication.”
What’s Next?
Scientists are working on solutions. The USDA’s Agricultural Research Service has developed CRISPR-edited grapefruit with 90% less furanocoumarin. Early trials show it’s safe and tastes the same. But it’s still years away from grocery stores.
In the meantime, the safest choice is simple: if your medication interacts with grapefruit, don’t drink it. Swap it for orange juice, water, or tea. Your body will thank you.
Can I drink grapefruit juice if I take my medication at night?
No. The enzyme-blocking effect lasts 24 to 72 hours after you drink grapefruit juice. Even if you take your pill at night and drink juice in the morning, your body still can’t properly break down the drug. The interaction isn’t about timing-it’s about the lasting damage to your gut enzymes.
Is grapefruit juice safe with blood pressure meds?
Some are, some aren’t. Felodipine and nifedipine can become dangerously strong when mixed with grapefruit juice, raising your risk of low blood pressure, dizziness, or heart issues. Amlodipine, however, is generally safe. Always check your specific drug’s label or ask your pharmacist.
Does grapefruit affect all statins the same way?
No. Simvastatin is the most dangerous-just one glass can triple its levels. Atorvastatin has a smaller effect, about 1.3 times higher concentration. Pravastatin and rosuvastatin show no significant interaction. If you’re on simvastatin and love grapefruit, talk to your doctor about switching to a safer statin.
Are there any citrus fruits I can safely drink with my meds?
Yes. Sweet oranges (navel, Valencia), lemons, and limes (Persian) do not contain the harmful chemicals found in grapefruit and Seville oranges. You can safely drink orange juice or lemon water with your medications. Avoid pomelos and Seville orange products like marmalade.
What if I accidentally drank grapefruit juice with my medication?
Don’t panic, but don’t ignore it either. If you’re on a high-risk medication like simvastatin, cyclosporine, or amiodarone, watch for symptoms like unexplained muscle pain, weakness, dark urine, dizziness, or irregular heartbeat. Call your doctor or pharmacist right away. They can advise if you need monitoring or a dose adjustment.


Comments
Babe Addict
Bro this is all just pharma fearmongering. CYP3A4 isn’t some magic off-switch - your liver’s got backup enzymes, and most people metabolize fine. I’ve been drinking grapefruit juice with my statin for 7 years and my CK levels are normal. They just want you to buy their ‘safe’ alternatives that cost 3x more.
On December 27, 2025 AT 10:50
Anna Weitz
It’s not about the juice it’s about control the system wants you scared of your breakfast so you’ll take their branded pills with their branded warnings and never question why your body can’t handle a fruit that’s been eaten for centuries
On December 29, 2025 AT 04:06
Elizabeth Alvarez
Have you ever wondered why the FDA and Big Pharma push this grapefruit myth so hard while quietly funding CRISPR research to eliminate furanocoumarins in citrus? It’s not about safety - it’s about creating dependency. They know if you can just edit the fruit to be safe, people will stop buying their expensive modified statins. The whole ‘24-72 hour window’? A distraction. The real danger is the patent cliff they’re trying to delay. They’ve been testing gene-edited grapefruit since 2018 and suppressing the results because they don’t want you to realize you can fix the problem without buying another prescription.
On December 30, 2025 AT 00:15
dean du plessis
Interesting read. I take amlodipine and drink grapefruit juice every morning. Never had an issue. But I also don’t take anything else that’s even close to the list. Maybe the real lesson is know your meds and know your body. Not all of us are the same. I’ve seen people panic over things that just don’t affect them. Chill. Check your label. Move on.
On December 30, 2025 AT 07:36
Paula Alencar
It is imperative that we, as conscientious consumers of pharmaceutical interventions, recognize the profound physiological implications of dietary interactions with pharmacokinetic pathways. The inhibition of CYP3A4 enzymatic activity within the enterocytes of the small intestine is not a trivial matter, but rather a clinically significant perturbation that may precipitate life-threatening adverse events, particularly among geriatric populations with polypharmacy. One must exercise due diligence in consulting with licensed pharmacists and reviewing the FDA-mandated prescribing information to mitigate risk. This is not a suggestion - it is a medical imperative.
On December 31, 2025 AT 14:17
Gerald Tardif
Man, I used to chug grapefruit juice with my Zocor like it was Gatorade. Then I started getting this weird muscle ache - didn’t think much of it until my doc said, ‘Dude, did you eat grapefruit?’ Turned out I was one of those 0.44 cases per 100 person-years. Switched to rosuvastatin. No more juice. No more pain. Life’s better now. Don’t be me.
On December 31, 2025 AT 21:50
Monika Naumann
Western medicine continues to weaponize fear against natural foods. In India, we have consumed citrus for millennia without such hysteria. This is a manufactured crisis designed to enrich multinational pharmaceutical corporations. Our ancestors did not need CRISPR-edited fruit - they needed wisdom, not warnings.
On January 1, 2026 AT 11:41
Elizabeth Ganak
so i just switched from simvastatin to pravastatin last month and now i can have my grapefruit again 😍 thanks for the clear breakdown! i was so scared to give up my morning juice but now i feel like i can breathe again
On January 1, 2026 AT 16:29
Raushan Richardson
YES. This is the kind of info we need. Not just ‘don’t drink it’ - but here’s what’s safe, here’s what’s not, and here’s how to talk to your pharmacist. I printed this out and gave it to my mom. She’s 72, takes 6 meds, and drinks grapefruit juice every day. She’s now switching to orange juice and says she feels like she just got a superpower.
On January 2, 2026 AT 01:47
Robyn Hays
What blows my mind is how many people think ‘natural’ means ‘safe’ - and then act like the body is some magic box that just ignores chemistry. Grapefruit doesn’t care if it’s organic or fair-trade. Those furanocoumarins don’t take a day off. I love citrus, but I’ve swapped grapefruit for blood oranges and lemon-ginger tea. My liver thanks me, and honestly? The tea tastes better anyway.
On January 3, 2026 AT 03:31
Liz Tanner
Just wanted to say: if you're on cyclosporine or amiodarone, please don't gamble with this. I had a cousin who ignored the warning, drank a glass of juice with her transplant med, and ended up in the ICU with acute kidney failure. She survived, but lost 30% of her kidney function. This isn't a ‘maybe.’ It's a ‘definitely don’t.’
On January 3, 2026 AT 07:33
Satyakki Bhattacharjee
People worry about juice but they take 10 pills a day with soda and candy. The real problem is not grapefruit - it’s that we treat our bodies like machines we can break and fix with more pills
On January 5, 2026 AT 03:19
Kishor Raibole
While the empirical evidence presented in this treatise is methodologically sound and corroborated by peer-reviewed literature from institutions of repute, one must nevertheless interrogate the epistemological foundations of pharmaceutical hegemony. The narrative of ‘avoid grapefruit’ is not merely a pharmacological advisory - it is a sociopolitical construct designed to reinforce the biopower of institutional medicine over the corporeal autonomy of the individual. To surrender one’s breakfast to corporate dictate is to surrender one’s sovereignty. The CRISPR grapefruit is not a solution - it is a Trojan horse. True liberation lies not in edited fruit, but in the rejection of the pharmacological paradigm itself.
On January 6, 2026 AT 06:55