When you need an antibiotic, a medicine used to treat bacterial infections. Also known as antibacterial agents, these drugs save lives—but only if you can actually get them. Too often, people face delays, high costs, or outright shortages. It’s not just about prescriptions being hard to fill—it’s about how global supply chains, overuse, and policy gaps make access uneven across communities.
Antibiotic resistance, when bacteria evolve to survive drug treatment is making this worse. Doctors can’t prescribe antibiotics that won’t work. That means even common infections like urinary tract infections or sinusitis might need stronger, more expensive, or harder-to-find drugs. And when those run out? You’re stuck waiting. Meanwhile, generic antibiotics, the cheaper, equally effective versions of brand-name drugs are often the solution—but they’re not always stocked, especially in rural pharmacies or low-income areas.
Why does this happen? Some manufacturers stop making cheap generics because profits are slim. Others face FDA delays or raw material shortages. In the U.S., a single antibiotic shortage can ripple through hospitals and clinics for months. And while you might think your doctor can just write a new script, many alternatives aren’t covered by insurance—or they come with side effects you can’t afford to risk.
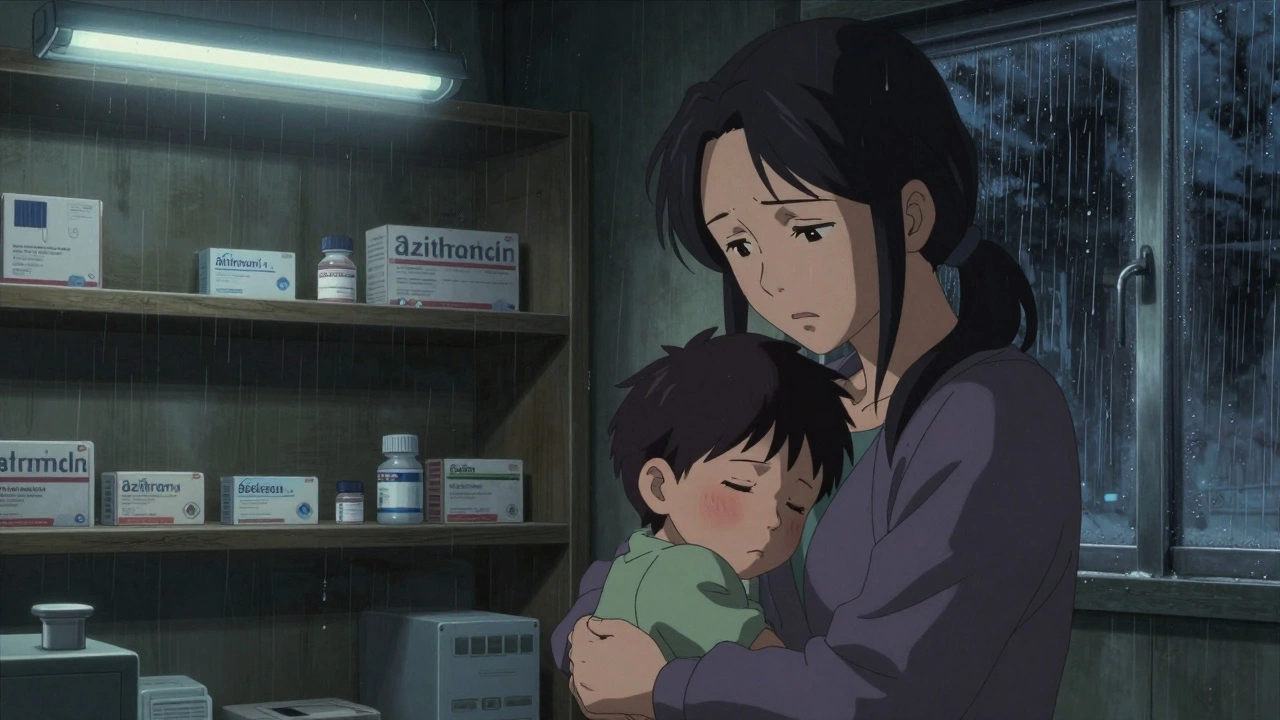
This isn’t just a healthcare problem. It’s a fairness issue. People without good insurance, transportation, or time off work suffer the most. A child with an ear infection shouldn’t have to wait days because the pharmacy ran out of amoxicillin. An elderly person with pneumonia shouldn’t be turned away because the local clinic only has one type of antibiotic left.
What can you do? Know your options. Ask your provider if a generic version is available. Check if your pharmacy participates in discount programs. Don’t pressure your doctor for antibiotics if they’re not needed—but don’t accept a delay if you clearly need one. And if you’ve had trouble getting antibiotics before, keep a list of what worked (and what didn’t) for next time.
The posts below cover real stories and facts about how antibiotics are regulated, why some drugs disappear from shelves, how patients fight for access, and what alternatives exist when the usual options fail. You’ll find guides on how to spot counterfeit antibiotics, how to talk to your pharmacist about shortages, and why the FDA sometimes blocks imports that look safe but aren’t. There’s also advice on what to do when you’re told "there’s nothing we can do"—and how to push back safely.
Antibiotic shortages are delaying treatment for common infections worldwide, forcing doctors to use riskier drugs or send patients home untreated. Rising resistance and broken economics are driving the crisis.
Read More© 2026. All rights reserved.