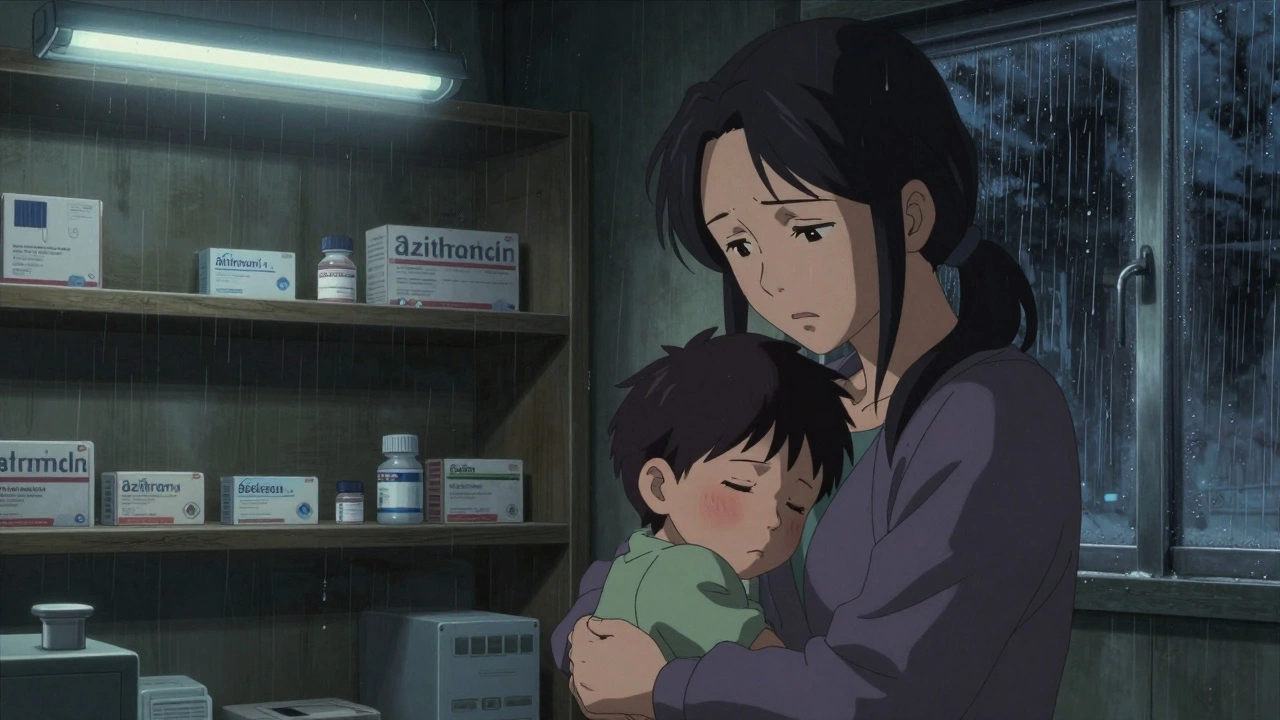
When antibiotic shortages, a sudden lack of essential medicines needed to treat common infections. Also known as drug supply gaps, they happen when manufacturers can’t keep up with demand—or stop making a drug altogether. This isn’t just a pharmacy problem. It’s a family health problem. If your child gets an ear infection or you develop a urinary tract infection, and the usual antibiotic isn’t on the shelf, what do you do? You wait. You risk the infection getting worse. Or worse—you end up with a stronger, more expensive drug that might have worse side effects.
Generic drug supply, the backbone of affordable antibiotics in the U.S. is fragile. Most of the antibiotics you take are made overseas, often in just one or two factories. If one of them shuts down for inspections, has a quality issue, or runs out of raw materials, the whole country feels it. The FDA drug monitoring, the system meant to catch problems before they reach patients doesn’t always see them coming. Real-time tracking is limited, and when a shortage hits, it’s often too late to stop the ripple effect.
And it’s not just about running out of amoxicillin. When one antibiotic disappears, doctors are forced to use alternatives—some less effective, some more expensive, some with higher risks of side effects. That’s how antibiotic resistance, when bacteria evolve to survive drugs meant to kill them grows. Using the wrong antibiotic, or taking it too long because the right one isn’t available, pushes bacteria to adapt. The result? Infections that used to be easy to treat now need hospital stays, IV drugs, or worse.
What can you do? First, don’t pressure your doctor for antibiotics if they say you don’t need them. Viral infections like colds and flu don’t respond to antibiotics—and pushing for them when they’re not needed makes shortages worse. Second, if your prescription is suddenly unavailable, ask your pharmacist: Is there an authorized generic? Is there another brand that’s equivalent? The FDA keeps lists of these, and your pharmacist can help you find them. Third, keep track of your medications. If you’re on a long-term antibiotic course, ask your provider if there’s a backup option in case the first one runs out.
This isn’t about fear. It’s about awareness. The antibiotic shortages you hear about in the news aren’t abstract—they affect your kitchen table, your child’s school, your elderly parent’s medicine cabinet. The posts below show you exactly how these shortages happen, who’s responsible, what the FDA does (and doesn’t do), and how families are adapting. You’ll find real stories about people who missed doses because their drug was gone. You’ll learn how Indian manufacturers keep the U.S. stocked, why some generics get pulled, and how to avoid dangerous substitutions. You’ll also see how skipping doses turns a simple infection into a life-threatening one. This isn’t theoretical. It’s happening right now. And you have more power to protect your family than you think.
Antibiotic shortages are delaying treatment for common infections worldwide, forcing doctors to use riskier drugs or send patients home untreated. Rising resistance and broken economics are driving the crisis.
Read More© 2026. All rights reserved.