Ever started a new medication and wondered if that weird headache, muscle ache, or stomach upset was the drug-or just bad luck? You’re not alone. Many people assume side effects show up right away, but that’s not always true. Some hit within hours. Others creep in weeks or even months later. Knowing when side effects typically start for different drugs can help you spot real problems faster-and avoid unnecessary panic or stopping meds too soon.
Why Timing Matters More Than You Think
It’s easy to blame a new pill for any symptom that pops up after you start taking it. But many conditions-like fatigue, dizziness, or joint pain-happen naturally, even in healthy people. The real question isn’t just “Did this happen after the drug?” It’s “Did it happen at the right time?” That’s where time-to-onset (TTO) comes in. It’s not just a fancy term. It’s a clinical tool doctors and researchers use to tell if a side effect is actually caused by the drug. If symptoms appear way too early or way too late for a certain class of medication, it’s less likely to be the culprit. And if they show up right in the expected window? That’s a red flag worth paying attention to.Fast Onset: Hours to Days
Some side effects are like alarm clocks-loud and immediate. These usually come from drugs that trigger direct biological reactions, not slow buildup. Take ACE inhibitors, for example. If you’re on lisinopril or enalapril for high blood pressure, angioedema (swelling of the face, lips, or throat) can strike within hours. That’s because these drugs interfere with a chemical called bradykinin, which causes rapid swelling. But here’s the twist: for some people, that same swelling doesn’t show up until weeks or months later. It’s rare, but documented. If you get sudden swelling after six months on the drug, don’t assume it’s allergies. Talk to your doctor. Antibiotics like ciprofloxacin are another fast hitter. Peripheral neuropathy-tingling, burning, or numbness in hands and feet-shows up in about half of cases within just two days. Studies show women tend to feel it even faster than men. If you start feeling pins and needles after your first or second dose, it’s not just “getting used to it.” That’s your body’s signal. And then there’s acetaminophen. Overdose? Liver damage can hit in under 24 hours. That’s why taking more than recommended-even a few extra pills-is dangerous. Timing here is life-or-death.Mid-Range: Days to Weeks
This is where most people get confused. Symptoms show up after a few days or weeks, so they assume it’s something else: stress, aging, a virus. But many common drugs have predictable patterns here. Statins-like atorvastatin or simvastatin-are a classic example. Muscle pain or weakness? It usually starts within the first few weeks. But here’s the surprise: in one major study, people who thought they had statin-induced muscle pain felt better just as fast when they switched to a placebo. That’s the nocebo effect-expecting side effects makes you more likely to notice them. Still, if the pain is real and lasts more than a week, don’t ignore it. Get checked. Antiepileptic drugs like pregabalin and gabapentin? Dizziness, drowsiness, and swelling in the legs typically appear within the first week. In fact, over half of users report these symptoms in the first seven days. If you’re starting one and feel foggy or unsteady, it’s probably the drug-not your sleep schedule. For many antibiotics, side effects like diarrhea or yeast infections show up after a few days. That’s because they kill off good gut bacteria faster than your body can rebalance. It’s not a sign the antibiotic isn’t working-it’s a side effect of how it works.
Delayed Onset: Weeks to Months
This is the scary part. Some side effects hide in plain sight because they show up so late. Interferon beta-1a, used for multiple sclerosis, can cause peripheral neuropathy after an average of 526 days-almost a year and a half. Imagine taking a drug for months, feeling fine, then suddenly getting numbness in your toes. Your doctor might think it’s a new MS flare. But if you’ve been on interferon for over a year? It could be the drug. Natalizumab, another MS drug, has a median onset of 141 days for nerve-related side effects. That’s nearly five months. If you’ve been on it for four months and start feeling weak or clumsy, don’t brush it off. Drug-induced liver injury? It often takes about six weeks. If you’re on methotrexate, antibiotics like amoxicillin-clavulanate, or even some herbal supplements, and you start feeling unusually tired, your skin turns yellow, or your urine looks dark, get your liver checked. It could be delayed toxicity. And yes, even antidepressants like SSRIs can cause delayed side effects. Sexual dysfunction or emotional blunting might not show up until you’ve been on them for a month or more. That’s why doctors ask about side effects at follow-ups-not just at the first visit.What Makes Timing Different Across Drugs?
Not all drugs work the same way, and that’s why timing varies so much. Drugs that act directly on receptors-like ACE inhibitors or antibiotics-tend to cause fast reactions. Their effects are immediate. Drugs that change your body’s chemistry slowly-like statins or antiepileptics-build up over days or weeks. Their side effects follow that curve. Then there are idiosyncratic reactions. These are unpredictable. Your immune system might react to a drug only after repeated exposure. That’s why hepatitis from drugs like valproate or sulfonamides can take 30-100 days to show up. It’s not about dose. It’s about your body’s unique response. Even sex and genetics matter. Women tend to experience certain side effects faster than men. A 2025 study found women on ciprofloxacin developed nerve symptoms two days after starting-men took four. Genetic differences in how you metabolize drugs also play a role. That’s why some people get side effects on low doses, while others don’t.How Doctors Use This Info
Hospitals and clinics aren’t just guessing anymore. Electronic health records now flag potential side effects based on timing. At Mayo Clinic, using TTO-based alerts improved detection of adverse reactions by 22% after they rolled out the system in early 2022. The FDA and European Medicines Agency now require drug makers to analyze time-to-onset data before approval. If a drug causes liver damage at 40 days, that has to be in the label. That’s why you’ll see phrases like “may occur after several weeks of therapy” on some prescriptions. Pharmacovigilance teams at drug companies use statistical models-like the Weibull distribution-to predict when side effects are likely to appear. If a new drug shows a pattern of reactions at 18 days, they’ll warn doctors and patients upfront.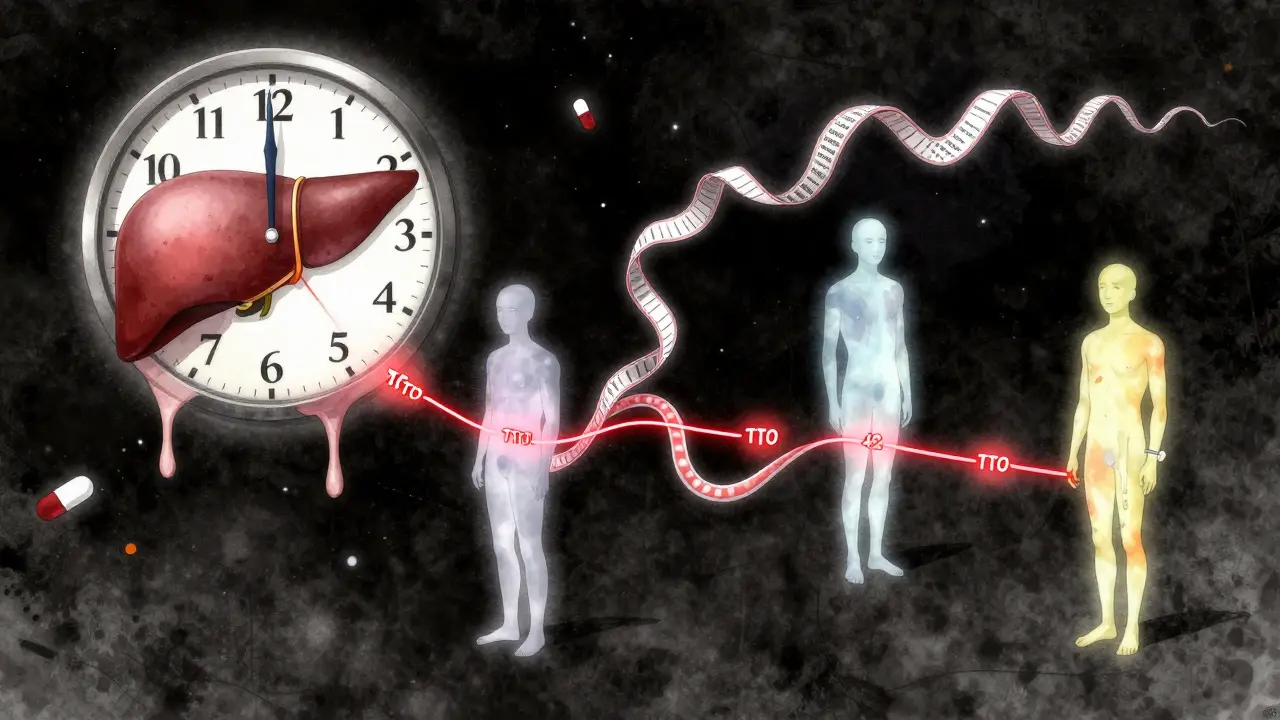
What You Can Do
You don’t need to be a doctor to use this info. Here’s how to apply it:- If you start a new drug, note the date. Write down any new symptoms and when they began.
- Compare your timeline to known patterns. If you got diarrhea on day 2 of antibiotics? That’s normal. If it’s on day 20? That’s unusual-call your doctor.
- Don’t assume everything is the drug. But don’t ignore symptoms that fit the known timing.
- Ask your pharmacist: “What side effects usually show up in the first week? What about after a month?”
- If a symptom disappears quickly after stopping the drug, it’s more likely to be drug-related. A 2021 study showed 55% of people with suspected statin side effects improved within 3 days of stopping-even if they were on placebo.
When to Worry
Not every new symptom means you need to stop your medication. But some red flags need immediate attention:- Swelling of the face, lips, tongue, or throat (angioedema)-call 999 or go to A&E immediately.
- Sudden yellowing of skin or eyes, dark urine, or extreme fatigue-could be liver damage.
- Unexplained muscle pain with weakness or dark urine-rhabdomyolysis risk.
- Numbness, tingling, or burning that spreads or gets worse-possible nerve damage.
The Bigger Picture
This isn’t just about avoiding bad reactions. It’s about using drugs safely and effectively. If you stop a drug too soon because you think a side effect is real-but it’s not-you might miss out on life-saving benefits. On the flip side, ignoring a delayed reaction because you think “it’s too late to be the drug” can lead to serious harm. The future is getting smarter. By 2025, the NIH’s All of Us program will start using genetic data to predict your personal time-to-onset risk. Wearables might soon track subtle changes in your heart rate or movement to flag early signs of side effects before you even notice them. But for now, the best tool you have is awareness. Know your meds. Know your timing. And don’t be afraid to ask questions.How soon after starting a drug do side effects usually appear?
It depends on the drug. Some side effects start within hours-like angioedema from ACE inhibitors. Others appear in days, like muscle pain from statins or tingling from ciprofloxacin. Some take weeks, like liver damage from certain antibiotics, and others may not show up until months later, such as nerve damage from interferon. There’s no single answer, but each drug class has a typical window.
Can a side effect start months after I begin taking a medication?
Yes. While many side effects appear early, some are delayed. For example, peripheral neuropathy from interferon beta-1a can take over a year to develop. Drug-induced liver injury often shows up between 3 and 12 weeks. Even angioedema from ACE inhibitors can occur after six months. If you develop a new symptom months into treatment, don’t rule out the medication-especially if it’s a known delayed reaction.
Are women more likely to experience side effects sooner than men?
For some drugs, yes. A 2025 study found women on ciprofloxacin developed peripheral nerve symptoms in 2 days, while men took 4 days on average. This is likely due to differences in metabolism, body composition, and hormone levels. Women also tend to report side effects more frequently overall, but timing differences are real and documented for specific drugs.
If my side effect goes away after stopping the drug, does that mean it was caused by the drug?
It’s a strong clue, but not proof. Many people feel better within days of stopping a drug-even if they were taking a placebo. That’s called the nocebo effect. Still, if symptoms disappear quickly after stopping and return when you restart (under medical supervision), that’s a much clearer sign the drug was the cause.
Should I stop my medication if I get a side effect?
Never stop a prescribed medication without talking to your doctor first. Some side effects are mild and go away on their own. Others are serious but treatable. Stopping suddenly can be dangerous-for example, stopping blood pressure or seizure meds abruptly can cause rebound effects. Always report the symptom, note when it started, and let your doctor decide the next step.
Do electronic health records track when side effects happen?
Yes. Systems like Epic and Cerner now include algorithms that flag potential drug reactions based on timing. For example, if a patient develops fatigue 45 days after starting methotrexate, the system may prompt the doctor to consider drug-induced liver injury. Mayo Clinic reported a 22% increase in detecting these reactions after adding TTO-based alerts in 2022.


Comments
Solomon Ahonsi
This whole post is just a fancy way of saying 'read the damn label.' I've been on statins for 3 years and my legs feel like lead. No one told me it could take weeks. Now I'm just mad I didn't quit sooner.
On February 3, 2026 AT 10:07